Eye Condition
Dry Eyes
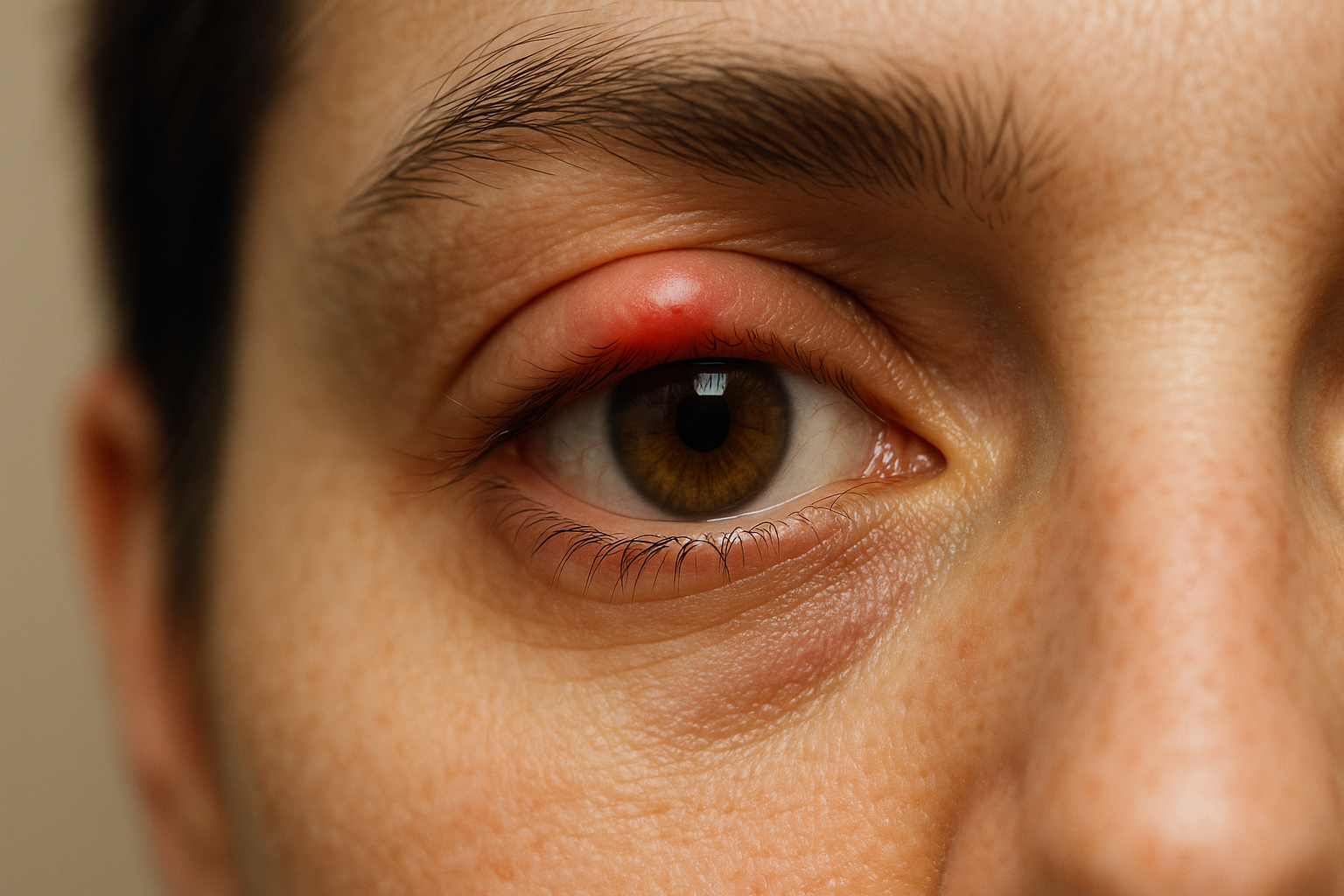
Dry eye disease is a common condition where inadequate or poor-quality tears leave the eyes feeling gritty, burning, and watery, potentially blurring vision and harming the cornea.

Explore our treatment options for Dry Eyes
What is Dry Eyes?
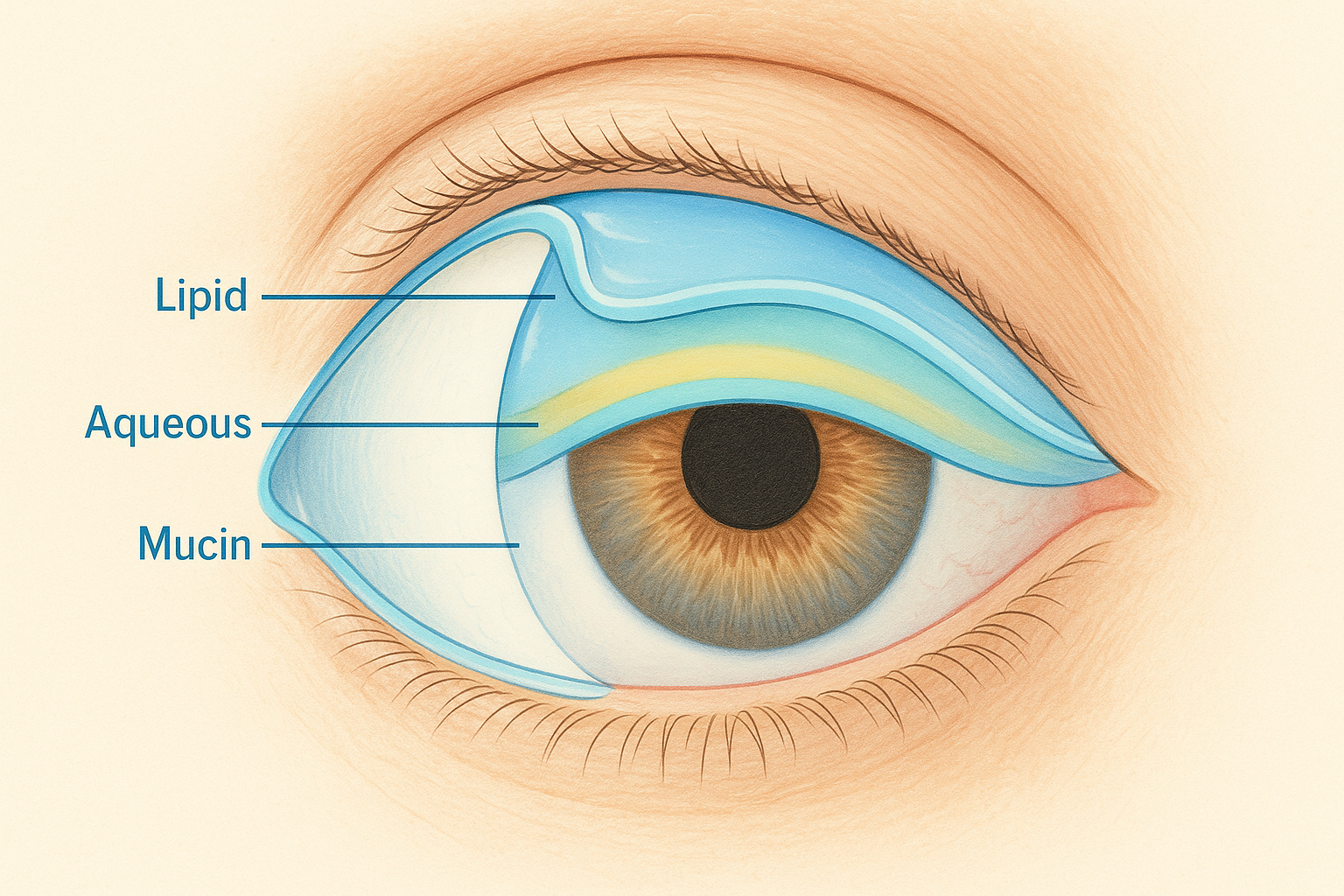
Dry eye disease (keratoconjunctivitis sicca) happens when your tears are too few or evaporate too quickly, leaving the eye surface without the moisture and nutrients it needs. Healthy tears form a clear, lubricating film that bathes the cornea every time you blink. When that film breaks down, you may feel stinging, itchiness, or see fluctuating vision. Although often thought of as a minor annoyance, persistent dryness can inflame the front of the eye, raise infection risk, and even scar the cornea over time. At the Eye Health Institute (EHI) we view dry eyes both as a local ocular issue and as a possible sign of wider systemic imbalance that deserves holistic attention.
Key symptoms and early warning signs
- Scratchy, sandy, or gritty feeling
- Eyes that water excessively after a period of dryness
- Sensitivity to wind, smoke, or air conditioning
- Blurry vision that clears after blinking
- Red, painful eyes or sudden light sensitivity
- Discomfort while reading, using screens, or driving at night
How Dry Eyes is diagnosed
During a comprehensive eye exam your doctor may:
- Ask detailed questions about symptoms, environment, and medications.
- Examine the tear film with a slit-lamp microscope and vital dyes (fluorescein, lissamine green) to reveal dry spots.
- Measure tear break-up time (TBUT) to see how long the tear layer remains stable.
- Use Schirmer strips or phenol red threads to gauge tear volume.
- Check the oil-producing meibomian glands of the lids.
- Review systemic factors such as thyroid disease, hormone shifts, or autoimmune disorders like Sjogren’s syndrome.
Why it happens: causes and risk factors
Dry eyes rarely stem from a single cause. Contributing factors include:
- Aqueous deficiency – the lacrimal glands underproduce the watery layer of tears. This is common with age, contact lens wear, certain antihistamines, and autoimmune conditions.
- Evaporative stress – blockages in meibomian glands thin the protective oil layer so tears evaporate faster. Digital screens, low-humidity offices, and blepharitis aggravate the problem.
- Systemic imbalance – Traditional East Asian medicine links ocular dryness to overall fluid and blood deficiency. Clinically we often see correlations with brittle nails, dry skin, joint stiffness, and digestive weakness. Autoimmune diseases such as rheumatoid arthritis or lupus may inflame the tear glands. Hormonal shifts in menopause, thyroid dysfunction, and imbalanced omega-3 intake can further tip the scales.
- Environmental triggers – smoke, wind, heating vents, and allergens irritate the ocular surface.
For a deeper medical overview, see the National Eye Institute’s patient guide on dry eye disease.
Conventional treatment options
Mainstream care focuses on replacing or conserving tears and controlling inflammation:
- Preservative-free artificial tears or gel drops used multiple times daily
- Lubricating ointment at night for severe cases
- Warm compresses and lid hygiene to improve meibomian gland flow
- Prescription anti-inflammatory eye drops (cyclosporine, lifitegrast)
- Low-dose oral doxycycline or azithromycin for lid inflammation
- Punctal plugs or thermal punctal cautery to slow tear drainage
- Scleral or moisture retention contact lenses that vault the cornea
These measures can give important relief but may not address underlying imbalances that drive chronic dryness.
Eye Health Institute’s integrative approach
EHI combines targeted ocular therapies with whole-body support to improve tear quality and comfort:
- Micro Acupuncture 48 & electro-acupuncture stimulate nerve pathways linked to lacrimal and meibomian gland function, aiming to boost natural tear production and reduce inflammation.
- Advanced microcurrent (ACS-3000) delivers gentle currents around the lids to encourage healthy oil secretion and calm irritated nerves.
- Customized botanical and nutritional plans emphasize omega-3 rich foods, anti-inflammatory herbs, and key micronutrients such as vitamins A, D, and gamma-linolenic acid to nourish the tear film.
- Hydrogen-rich water and topical hydrogen mist are offered in-clinic to combat oxidative stress at the ocular surface.
- Lifestyle coaching covers workspace humidity, screen ergonomics, eye-blinking drills, and stress reduction techniques like breathwork or gentle qigong.
Our experience shows that many dry-eye patients notice softer lids, less burning, and steadier vision within the first several sessions. Ongoing home programs and periodic in-office “eye spa” maintenance help sustain comfort alongside any conventional therapy your ophthalmologist prescribes.
What patients report / clinical insights
Patients often arrive frustrated after cycling through numerous drops. Once the lid oils start flowing and systemic hydration improves, they describe:
- Faster tear break-up times documented by follow-up testing
- Ability to work at a computer or read longer without ache or blur
- Less dependence on artificial tears throughout the day
- Overall sense of improved vitality, noting that skin and joints feel less dry
While individual responses vary, integrating ocular therapies with systemic support broadens the pathway to lasting relief.

When to seek urgent care
Get urgent eye care right away if you experience any of the following:
- Sudden severe eye pain or pressure
- A new curtain or shadow across vision
- Many new floaters with light flashes
- Rapid loss of vision in one or both eyes
- Eye trauma or chemical splash
These symptoms may signal corneal infection, retinal detachment, or acute glaucoma and require immediate medical attention.