Eye Condition
Rod-Cone Dystrophy
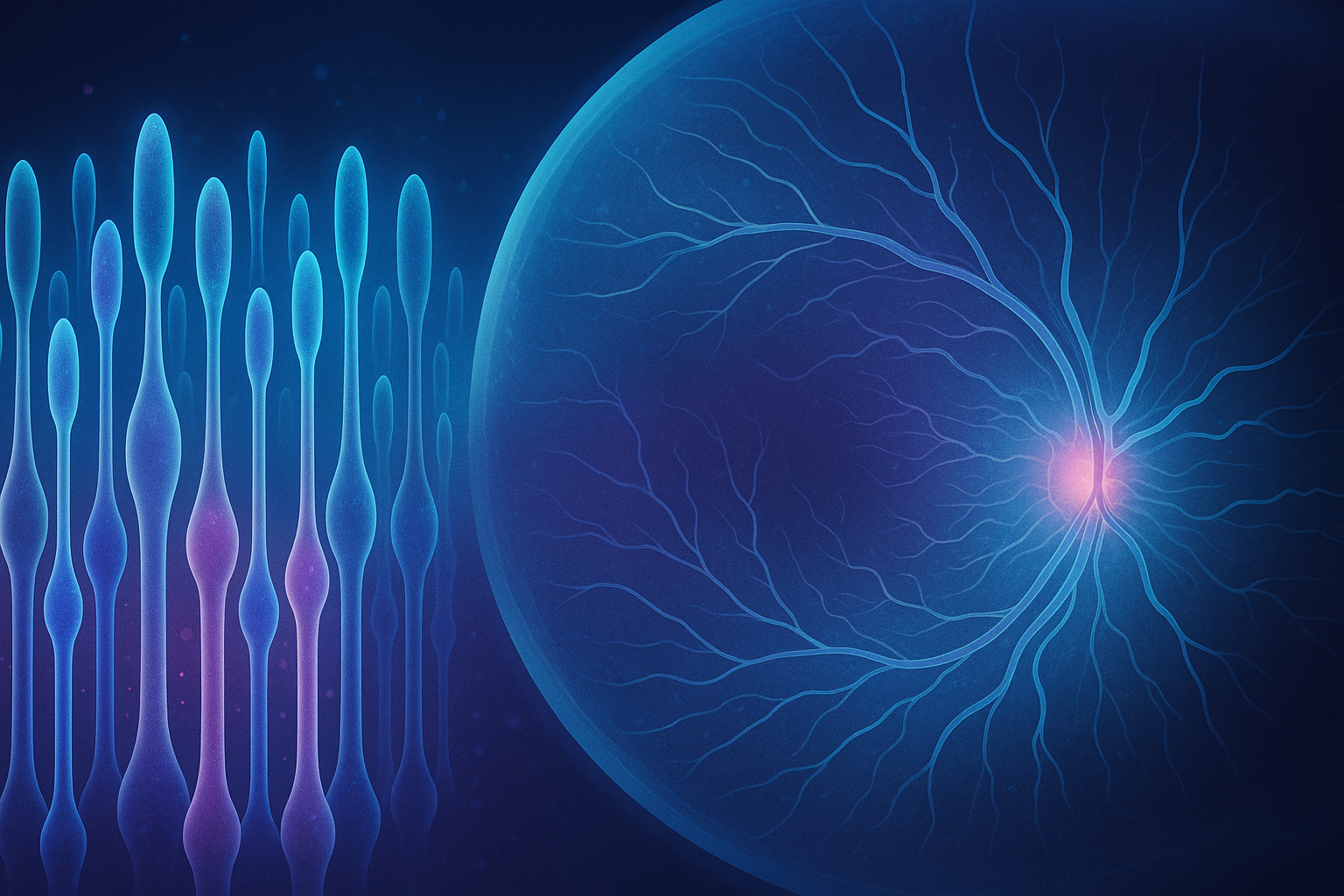
Rod-cone dystrophy is a genetic condition that causes progressive vision loss, often starting in childhood.
Explore our treatment options for Rod-Cone Dystrophy
What is Rod-Cone Dystrophy?
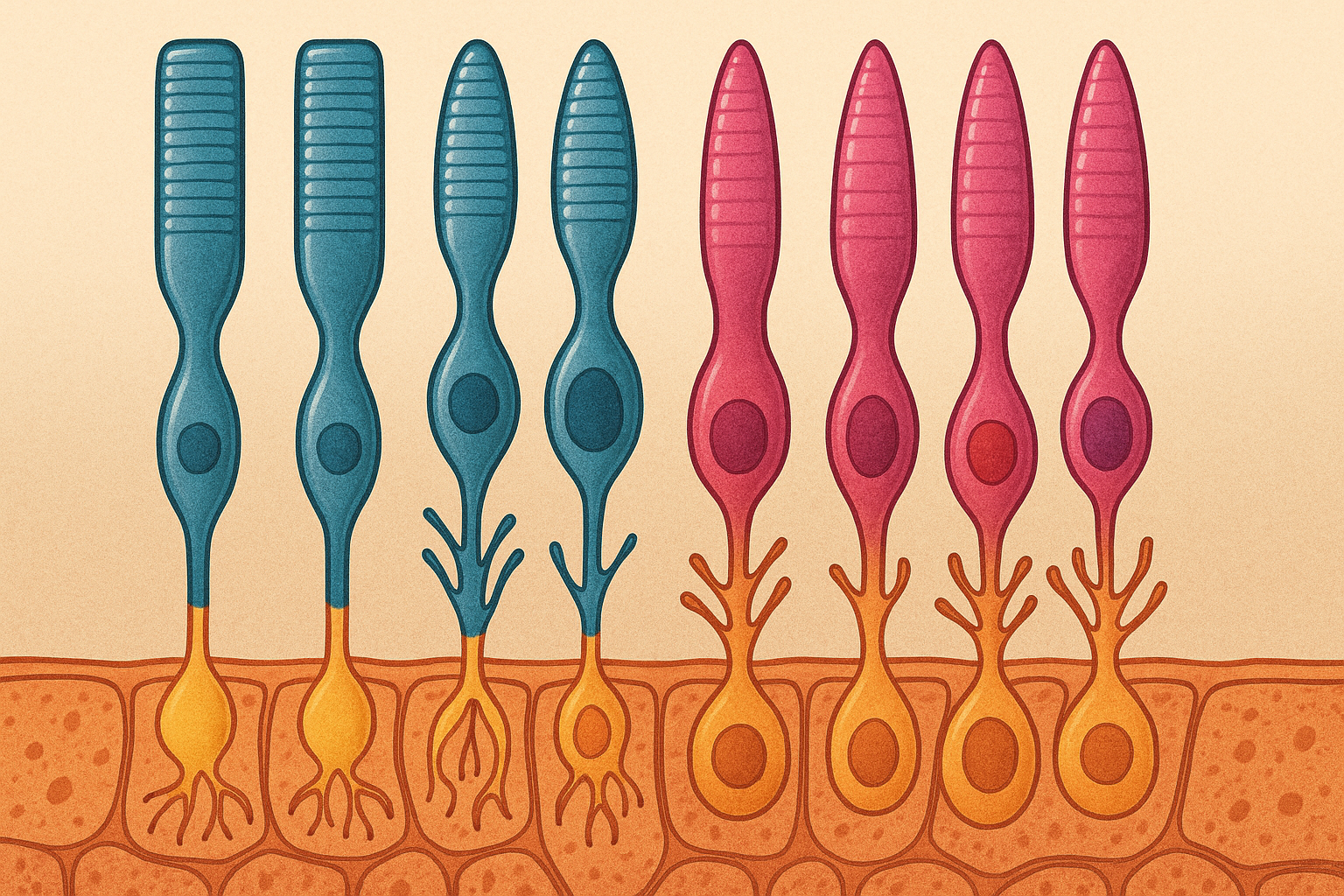
Rod-cone dystrophy is an inherited retinal disease that causes the light-sensing rod and cone cells to break down over time. Rods help you see in dim light, while cones provide sharp central vision and color perception. When these photoreceptors deteriorate, you may first notice trouble seeing at dusk, followed by changes in side vision, color discrimination, and, eventually, central clarity. Although it is rare, the condition can progress to legal blindness. Because rod-cone dystrophy affects people of all ages and often runs in families, early recognition gives you more options to protect the vision you still have.
Key symptoms and early warning signs
- Night blindness (trouble seeing in dim light or at dusk)
- Gradual loss of peripheral vision, creating a tunnel-like view
- Increasing difficulty telling colors apart, especially in low light
- Glare or light sensitivity
- New flashes or sudden shower of floaters – seek care right away
- In advanced stages, blurred or missing central vision that affects reading and face recognition
Because changes often start slowly, regular eye exams can detect early functional loss before you notice major day-to-day problems.
How Rod-Cone Dystrophy is diagnosed
Eye doctors begin with a detailed case history, including family eye health. Key tests may include:
- Electroretinography (ERG) – records the electrical responses of rods and cones to brief light flashes, revealing early dysfunction.
- Optical coherence tomography (OCT) – high-resolution cross-section images show thinning of retinal layers.
- Visual field testing – maps side vision loss and tracks progression over time.
- Genetic testing – pinpoints the specific mutation, offering clearer prognosis and helping relatives understand their own risk.
- Dark adaptation measurement – evaluates how quickly your eyes adjust from light to dark.
A precise diagnosis guides both conventional and integrative treatment planning.
Why it happens: causes and risk factors
Rod-cone dystrophy is most often caused by mutations in genes that keep photoreceptors healthy, similar to the broader group of inherited retinal diseases such as retinitis pigmentosa. More than 60 genes have been implicated, and the same gene can produce different degrees of severity in different families. While anyone can be affected, risk rises when:
- Close relatives have an inherited retinal condition
- You belong to a population with limited genetic diversity
- A systemic syndrome (for example Usher or Bardet–Biedl) is present
Researchers continue to investigate how oxidative stress, mitochondrial function, and inflammation influence the speed of degeneration.
Conventional treatment options
At this time, no approved drug or surgical cure exists. Standard care focuses on slowing vision loss, maximizing remaining sight, and supporting daily function:
- Low-vision rehabilitation and assistive technology
- Prescription sunglasses or photochromic lenses to control glare
- Nutritional counseling aimed at overall retinal health
- Clinical trial enrollment for emerging gene or cell therapies whenever appropriate
- Monitoring for secondary issues such as cataracts or macular edema
Working closely with a retinal specialist ensures timely updates on new research and interventions.
Eye Health Institute’s integrative approach
Dr. Andy Rosenfarb’s team combines Traditional Chinese Medicine, naturopathic strategies, and modern biophysical therapies to complement medical eye care:
- Micro Acupuncture 48 and classical acupuncture – targeted point protocols aim to improve ocular blood flow, modulate inflammation, and support retinal metabolism.
- Alternating Current Stimulation (ACS-3000 microcurrent) – gentle frequency-specific electrical pulses delivered around the eyes may help photoreceptor mitochondrial function and nerve signaling.
- Hydrogen therapy – inhalation or hydrogen-rich water tablets provide powerful antioxidant support that can neutralize damaging free radicals generated in degenerating retinas.
- Individualized herbal and nutritional programs – formulas rich in carotenoids, omega-3 DHA, and adaptogenic botanicals are selected based on genetic profile and systemic health.
- Guided lifestyle coaching – stress management, regular aerobic activity, balanced blood sugar, and blue-light hygiene all play roles in slowing degenerative change.
- Intensive in-office programs plus home protocols – many patients visit for a one-week or two-week intensive that combines daily therapies, then continue maintenance care at home using microcurrent devices and supplements.
These modalities are designed to support retinal cell energy, reduce oxidative stress, and optimize visual function. They work alongside your ophthalmologist’s medical plan rather than replacing it.
What patients report / clinical insights
Many patients describe sharper contrast, brighter colors, and a wider visual “window” after a course of integrative care, even when traditional testing shows only modest numeric change. Improvements are often most noticeable in:
- Confidence navigating at dusk or in movie theaters
- Recovery time when moving from bright to dim environments
- Reading endurance and digital screen comfort
- Overall eye comfort and reduction in visual fatigue
As with any chronic condition, outcomes vary. Consistent follow-up lets the team tailor treatment frequency and adjust home routines to keep your progress on track.

When to seek urgent care
Get urgent eye care if you experience sudden vision loss, a curtain-like shadow in your field of view, a burst of many new floaters with flashes of light, severe eye pain, or direct eye injury. These events can signal retinal detachment, hemorrhage, or acute inflammation that demands immediate treatment to prevent permanent damage.