Eye Condition
Sjogren's Syndrome
Sjogren’s syndrome is an autoimmune attack on tear glands, causing chronic dry, gritty eyes, fluctuating blur and redness.

Explore our treatment options for Sjogren's Syndrome
What is Sjogren’s Syndrome?
Sjögren’s syndrome (pronounced “SHOW-grins”) is a long-term autoimmune disorder in which the immune system attacks the body’s moisture-producing glands. When the tear glands are affected, the front surface of the eye loses its protective film of tears, leaving it exposed, irritated, and vulnerable to infection. Although dryness is the hallmark, this systemic condition can also involve joints, skin, nerves, and internal organs. At the Eye Health Institute (EHI), our focus is on protecting the ocular surface and supporting overall comfort with a blend of conventional and integrative therapies.
If you are already searching for relief from chronic Dry Eyes, understanding whether Sjogren’s is the underlying driver can be a key first step toward lasting solutions.
Key symptoms and early warning signs
- Persistent burning, gritty, or stinging eyes
- Fluctuating blurry vision that improves after blinking
- Light sensitivity, especially in windy or dry environments
- Redness that lingers after rest
- Dry mouth with trouble swallowing or speaking for long periods
- Swollen salivary glands near the jaw or ears
- Joint stiffness, morning aching, or generalized fatigue
- Skin dryness or rashes
Early treatment of ocular surface stress can help prevent corneal damage and reduce infection risk.
How Sjogren’s Syndrome is diagnosed
EHI uses a combination of in-office tests and laboratory work-ups to confirm the diagnosis and grade severity:
| Test | What it shows |
|---|---|
| Schirmer’s tear strip | Actual tear volume over 5 minutes |
| Ocular surface staining (fluorescein, lissamine green) | Areas where cells are damaged by dryness |
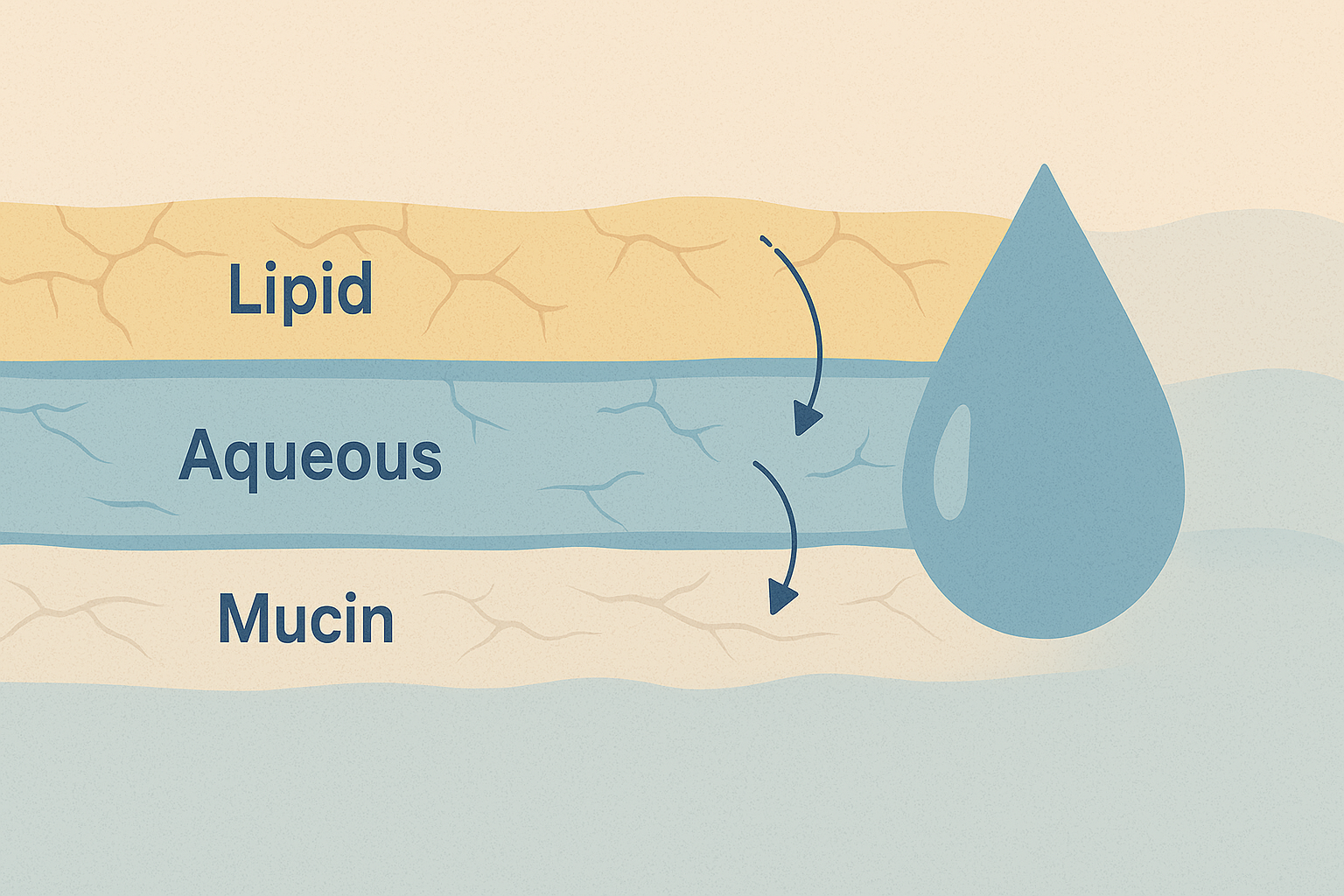
| Tear break-up time | Stability of the tear film before it evaporates |
| Blood panel (SSA/Ro, SSB/La antibodies) | Autoantibodies linked to Sjogren’s |
| Minor salivary gland biopsy | Confirms lymphocyte infiltration |
| Imaging (ultrasound of salivary glands) | Structural changes in exocrine tissue |
A rheumatology referral is common because systemic features often need coordinated care.
Why it happens: causes and risk factors
Researchers believe a mix of genetic predisposition, sex hormones, and environmental triggers (such as viral infections) flips the immune system into overdrive. The condition is most common in women over 40 and frequently coexists with other autoimmune diseases like rheumatoid arthritis or lupus. Certain medications, low-humidity workplaces, and lifestyle stressors can worsen ocular dryness even after the disease is diagnosed.
The National Eye Institute offers clear patient information that can help you track research progress and clinical trials on Sjogren’s-related dry eye; visit the National Eye Institute website for further reading.
Conventional treatment options
Mainstream therapy focuses on symptom relief and inflammation control:
- Preservative-free artificial tears, gels, and ointments
- Prescription anti-inflammatory eye drops (cyclosporine, lifitegrast)
- Punctal plugs or cautery to slow tear drainage
- Moisture chamber glasses and humidifier use
- Oral pilocarpine or cevimeline to stimulate saliva
- Systemic immunomodulators (hydroxychloroquine, methotrexate) for severe systemic disease
- Preventive dental care and sugar-free lozenges for the dry mouth component
Working with your ophthalmologist and rheumatologist ensures medications are optimized and monitored for side effects. Even with appropriate pharmaceuticals, many patients still experience day-to-day fluctuations, which is where supportive, lifestyle-based therapies can make a difference.
Eye Health Institute’s integrative approach
Because Sjogren’s is multifaceted, EHI builds a personalized plan that complements your medical regimen while addressing root contributors to dryness:
- Micro Acupuncture 48 and targeted electroacupuncture protocols to help modulate immune activity and support lacrimal gland function
- Gentle periocular microcurrent stimulation (ACS-3000) that aims to improve meibomian gland flow and tear stability
- Customized Chinese herbal formulas and evidence-informed nutraceuticals (omega-3s, vitamin A, turmeric) chosen for anti-inflammatory and mucosal-support properties
- Hydrogen inhalation sessions and topical antioxidant eye mists to combat oxidative stress on the ocular surface
- Guided lifestyle coaching on hydration strategies, anti-inflammatory nutrition, blue light hygiene, and stress reduction techniques such as qigong
- At-home follow-up kits with heat masks, compresses, and preservative-free tear samples to extend clinic benefits between visits
Our goal is not to replace your rheumatologist but to bridge the gap between systemic management and everyday visual comfort so you can read, drive, and work with fewer interruptions.
What patients report / clinical insights
Many people arrive feeling that standard lubricant drops give only minutes of relief. After intensives that combine acupuncture, microcurrent, and nutrition counseling, EHI patients often describe smoother blinking, less morning blurriness, and reduced dependence on rewetting drops. The relief may begin within days for some, but sustained gains usually follow a series of visits coupled with home care. Consistency and realistic expectations remain essential to long-term success.

When to seek urgent care
Get urgent eye care if you experience sudden vision loss, a curtain-like shadow across your sight, many new floaters with flashes of light, severe eye pain, or trauma to the eye. These can signal emergencies such as retinal detachment, infection, or acute inflammation that require prompt medical attention.