Eye Condition
Ocular Rosacea
Ocular rosacea is a chronic inflammatory disorder that irritates the eyelids and eye surface, and it is closely linked to the skin form of rosacea.
Explore our treatment options for Ocular Rosacea
What is Ocular Rosacea?
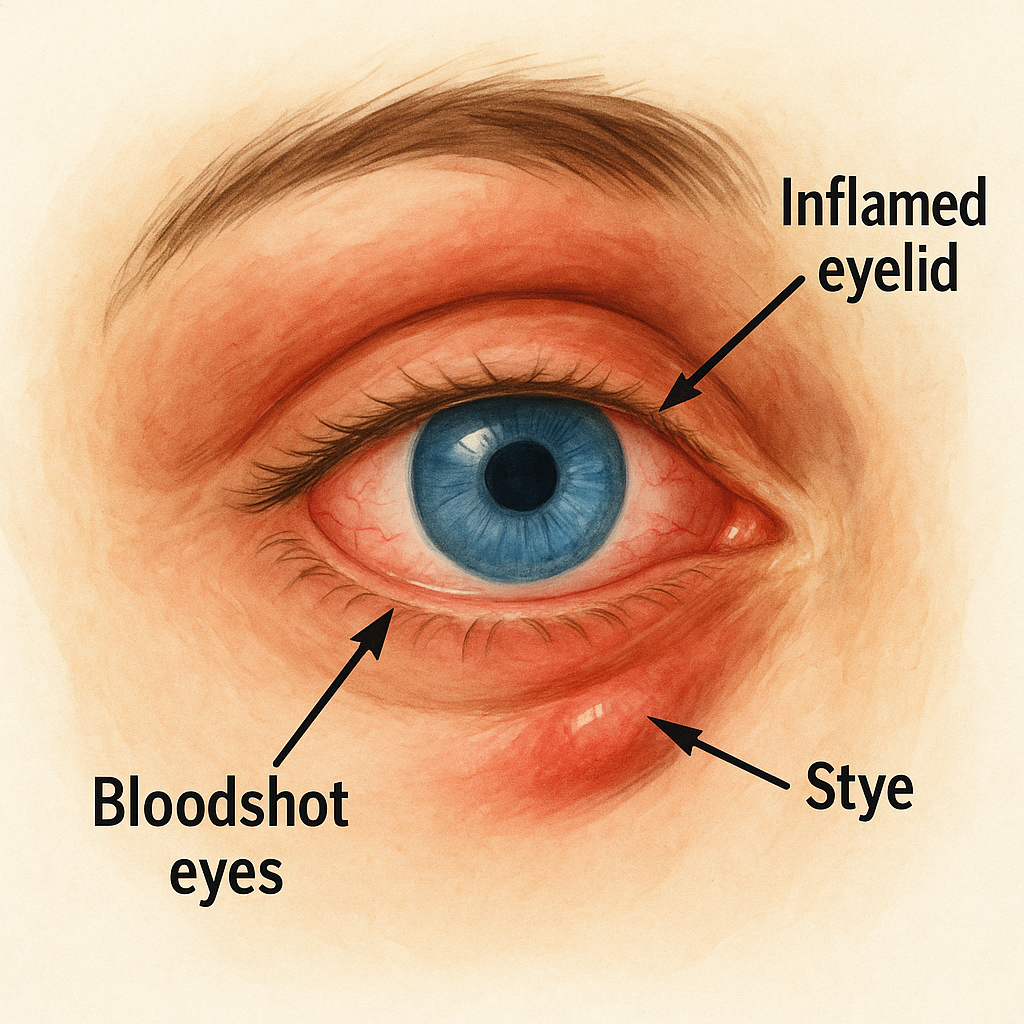
Ocular rosacea is a chronic inflammatory eye condition that often accompanies facial rosacea. It primarily affects the eyelids, meibomian glands, and the clear surface of the eye (conjunctiva and cornea). Persistent redness, burning, and a gritty sensation in and around the eyes can make everyday tasks uncomfortable. Without timely care, long-standing inflammation may damage the ocular surface and threaten sight, yet early diagnosis and a tailored treatment plan can ease symptoms and help safeguard vision.
Key symptoms and early warning signs
- Red, bloodshot appearance that does not clear with rest
- Burning or stinging pain
- Gritty, sandy feeling, especially on waking
- Swollen eyelid margins or crusting at the lashes
- Fluctuating or blurred vision that improves after blinking
- Sensitivity to wind, smoke, or bright light
- Dryness that resembles Dry Eyes
Recognizing these signs early allows you and your eye-care team to limit flare-ups and protect the corneal surface.
How Ocular Rosacea is diagnosed
An evaluation typically includes:
- Comprehensive slit-lamp exam of lids, lashes, conjunctiva, and cornea
- Meibomian gland expression to look for thickened oil secretions
- Tear film break-up time and ocular surface staining tests
- In-depth discussion of skin rosacea history, diet, environment, and medications
Pinpointing triggers and grading severity guides both medical and integrative treatment planning.
Why it happens: causes and risk factors
Researchers believe ocular rosacea stems from a combination of genetics, immune dysregulation, and environmental stressors that increase ocular surface inflammation. Factors that raise risk include:
- Existing facial rosacea, especially long-standing or severe cases
- Age over 30
- A family history of rosacea or related inflammatory conditions
- Hormonal changes and high environmental temperatures
- Demodex eyelash mites and bacterial overgrowth along the lids
- Diets high in spicy foods, alcohol, or refined carbohydrates
- Frequent screen use that reduces blinking and worsens tear evaporation
Conventional treatment options
Mainstream therapy focuses on reducing inflammation, improving meibomian gland function, and stabilizing the tear film. Your ophthalmologist may recommend:
- Warm compresses and lid massage to melt thickened oils
- Daily non-irritating eyelid cleansers to reduce bacterial load
- Prescription oral antibiotics such as low-dose doxycycline or azithromycin
- Topical anti-inflammatories or cyclosporine drops to calm immune activity
- Preservative-free artificial tears or gels for surface lubrication
- In-office therapies like thermal pulsation to unclog glands
Conventional measures often provide relief, yet some patients need multifaceted support to fully manage flares.
Eye Health Institute’s integrative approach
Drawing on Dr. Andy Rosenfarb’s experience with integrative ophthalmology, EHI blends evidence-informed therapies that complement your medical regimen and aim to soothe inflammation from the inside out.
Core modalities we may incorporate:
- Acupuncture and Micro Acupuncture 48 sessions targeting ocular surface circulation, lid gland output, and systemic immune balance
- Low-level microcurrent stimulation (ACS-3000) to promote cellular repair and nerve function around the eyelids
- Customized Chinese herbal formulas and nutraceuticals rich in omega-3 fatty acids, antioxidants, and anti-inflammatory compounds such as turmeric and quercetin
- Nutritional counseling that emphasizes whole foods, gut health, and reduced dietary triggers like alcohol and spicy dishes
- Moist heat eye masks, gentle gland expression, and “blink training” for patients who spend long hours on screens
- Stress management and breath-work to minimize flare-triggering cortisol spikes
Because ocular rosacea symptoms can ebb and flow with lifestyle, weather, and stress, we track progress closely and adjust protocols during on-site intensives or at-home programs. Many patients report fewer flares, improved comfort, and better tolerance of contact lenses once surface inflammation is tamed.
What patients report / clinical insights
Patients often describe waking with dry, crusted-over lids that feel as if “sand is trapped under the lashes.” After several weeks of combined lid hygiene, nutraceutical anti-inflammatories, and targeted acupuncture or microcurrent care, they commonly notice:
- Eyes feel less gritty throughout the day
- Makeup and contact lenses can be worn longer without irritation
- Flare frequency drops, especially during seasonal weather swings
- Skin rosacea triggers (hot drinks, stress, spicy meals) cause milder eye reactions
Our clinical observation is that consistent at-home lid care plus internal anti-inflammatory support make in-office treatments more effective and help sustain gains between visits.

When to seek urgent care
Get urgent eye care if you experience sudden vision loss, a curtain-like shadow, many new floaters with flashes, severe eye pain, intense light sensitivity that prevents opening the eye, or a non-healing corneal ulcer. These signs can indicate emergencies such as corneal infection or retinal involvement and require prompt attention to prevent permanent vision damage.