Eye Condition
Macular Pucker (Macular Hole)
Macular pucker (epiretinal membrane) is a thin scar layer on the macula that contracts, wrinkling the retina and blurring or distorting central vision.
Explore our treatment options for Macular Pucker (Macular Hole)
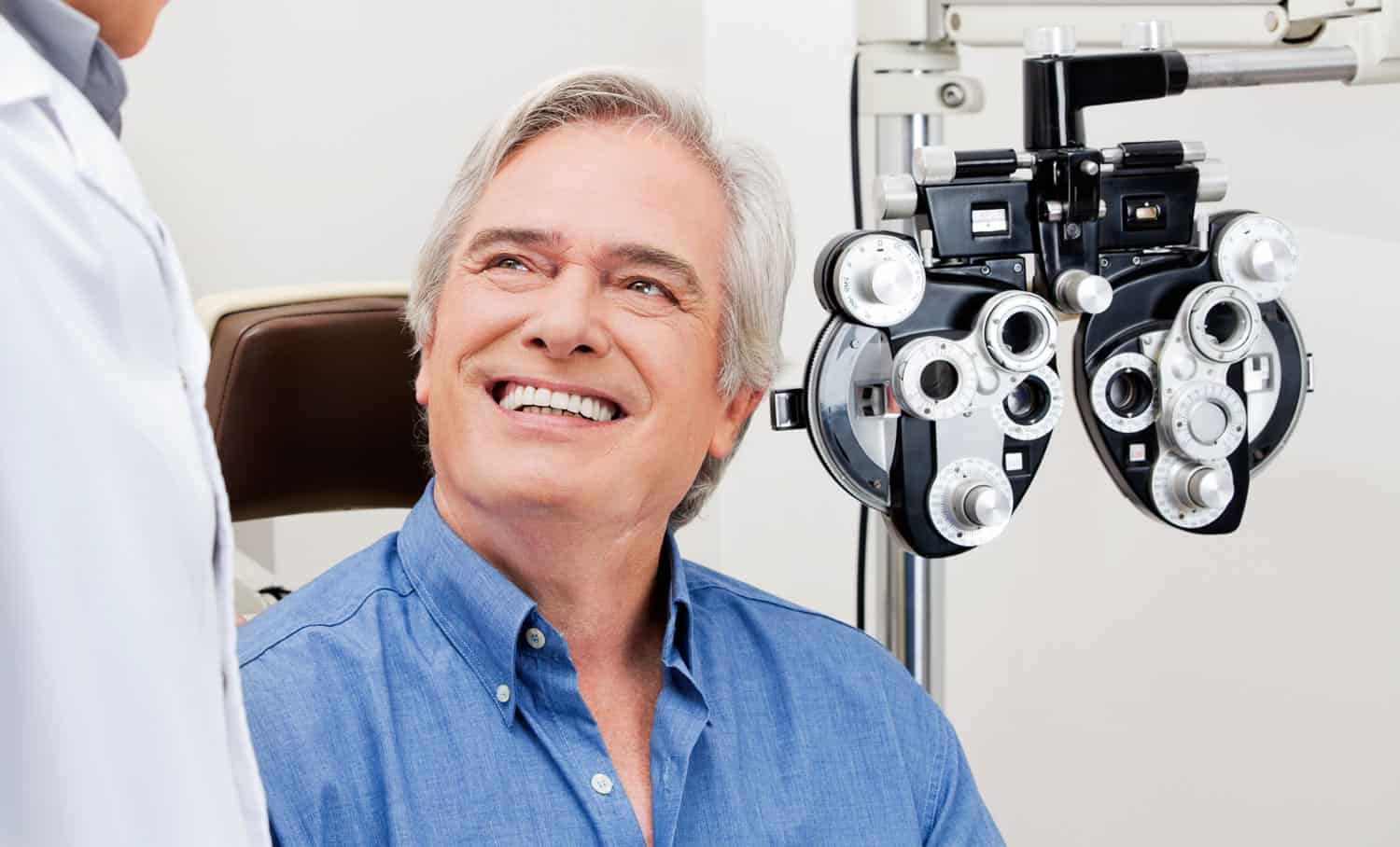
Overview
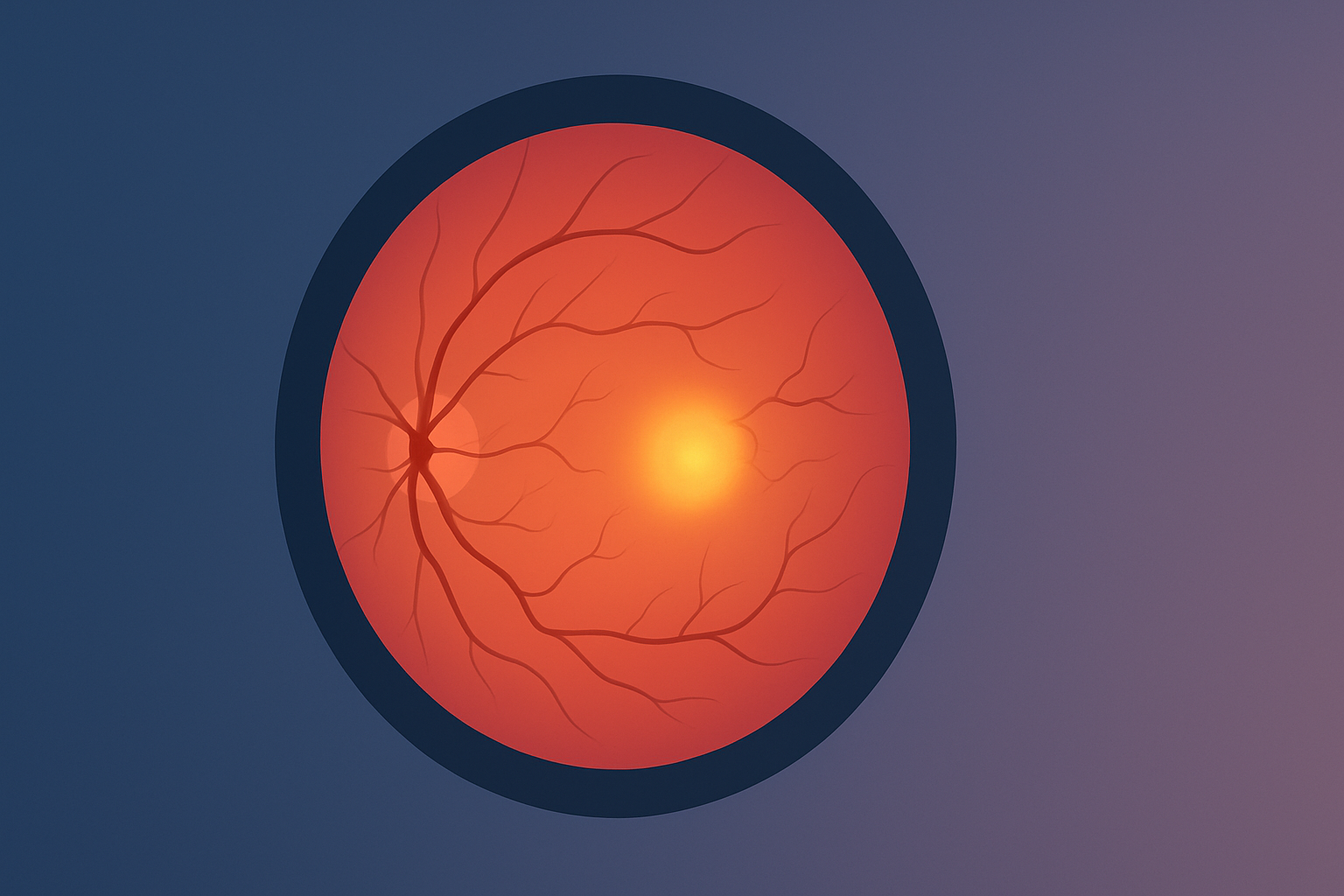
The macula is the pinpoint center of the retina that lets you read fine print, drive, and recognize faces.
Two common disorders can disturb this critical spot:
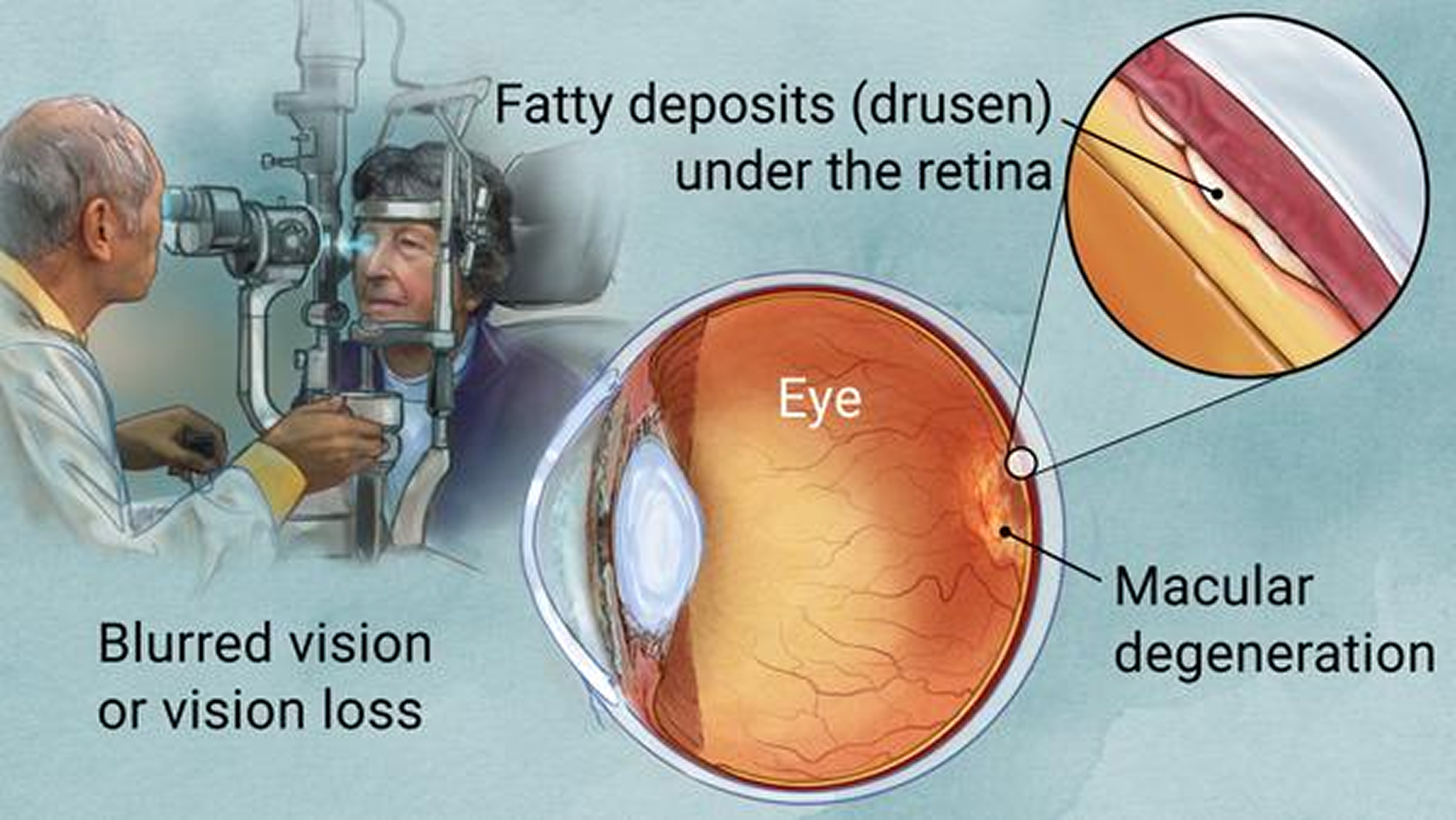
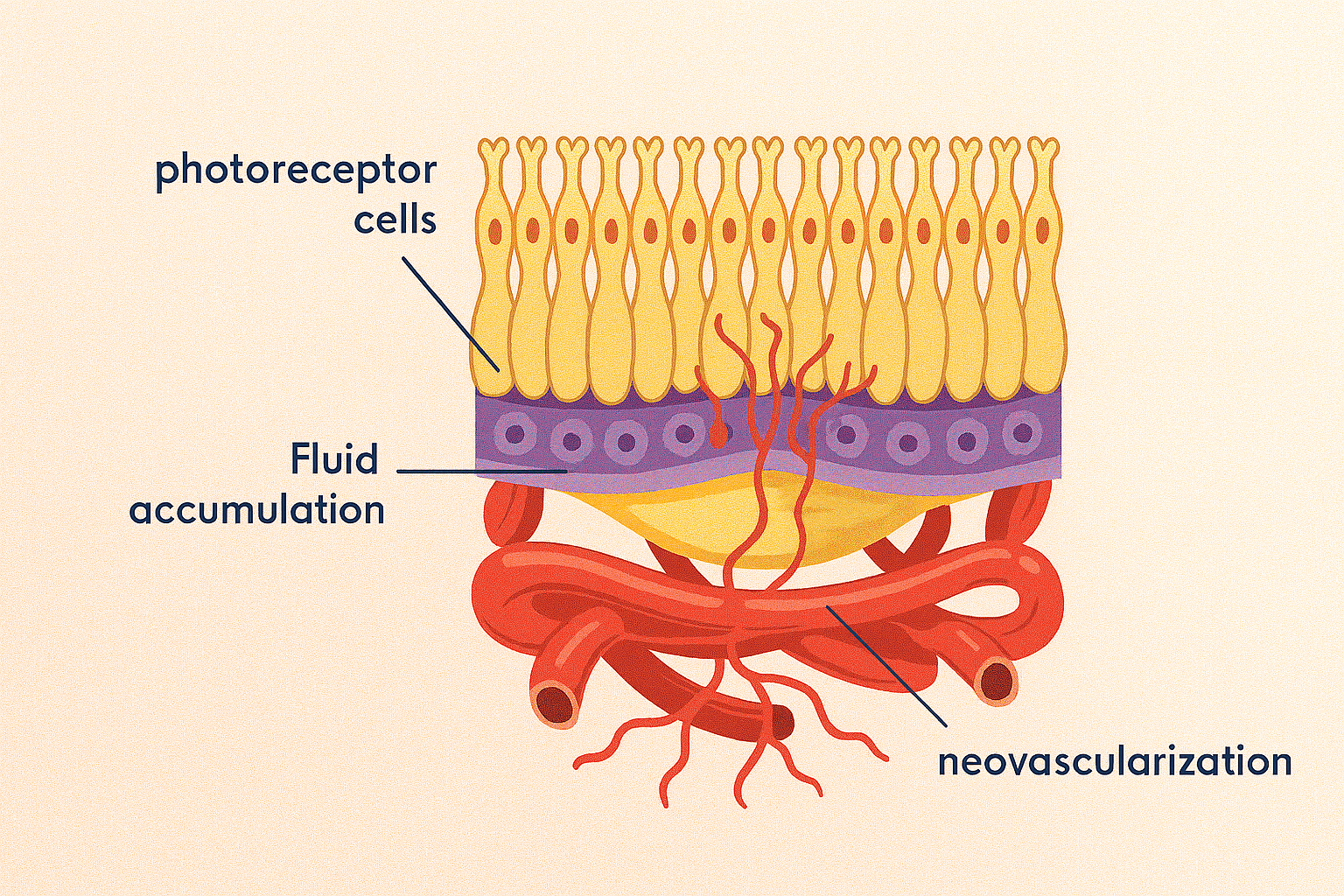
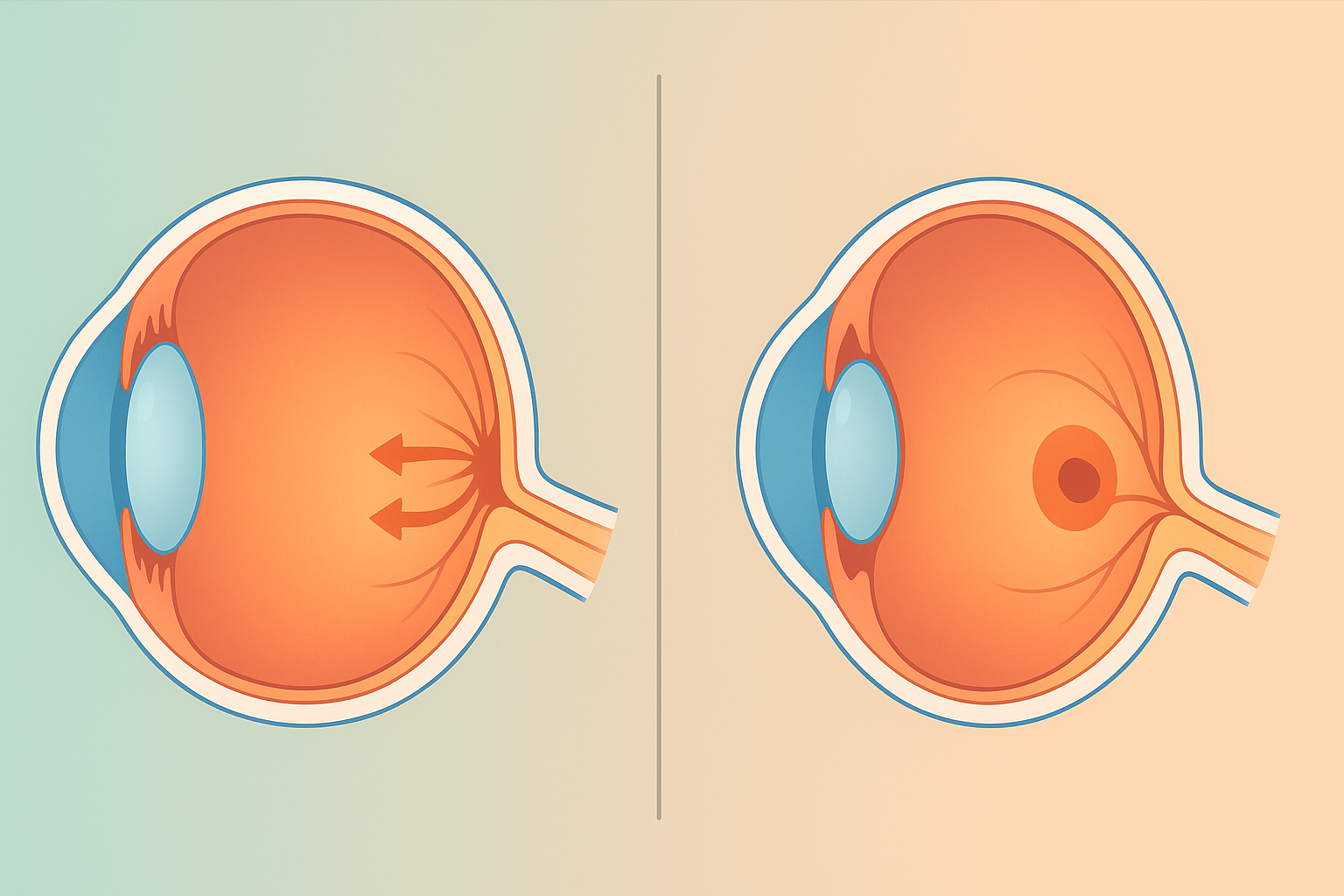
- Macular Pucker (Epiretinal Membrane): A paper‑thin, transparent layer of scar‑like tissue that grows on the macula and contracts, “wrinkling” the retinal surface. Central vision becomes blurry or distorted; straight lines look wavy.
- Macular Hole: A full‑thickness break through the macula, usually from age‑related traction between the vitreous gel and the retina. A gray or dark spot can form in the center of vision, causing drop‑off in clarity or complete loss if untreated.
Although both disrupt central sight, a pucker wrinkles the surface, while a hole punches through it. Modern imaging (OCT) can tell them apart in seconds, and timely surgery can often restore useful vision.
Macular Pucker (Epiretinal Membrane)
Causes & Risk Factors
- Aging vitreous shrinkage
- Retinal tears, inflammation, diabetic retinopathy
- Eye trauma or surgery
Signs & Symptoms
- Blurred or hazy central vision
- Straight lines appear bent
- Gray “cellophane” sheen over vision
Diagnosis
Dilated exam + OCT to show the crinkled membrane.
Treatment
Observation for mild cases; vitrectomy with membrane peel if distortion worsens (≈ 90 % improve ≥ 1–2 lines).
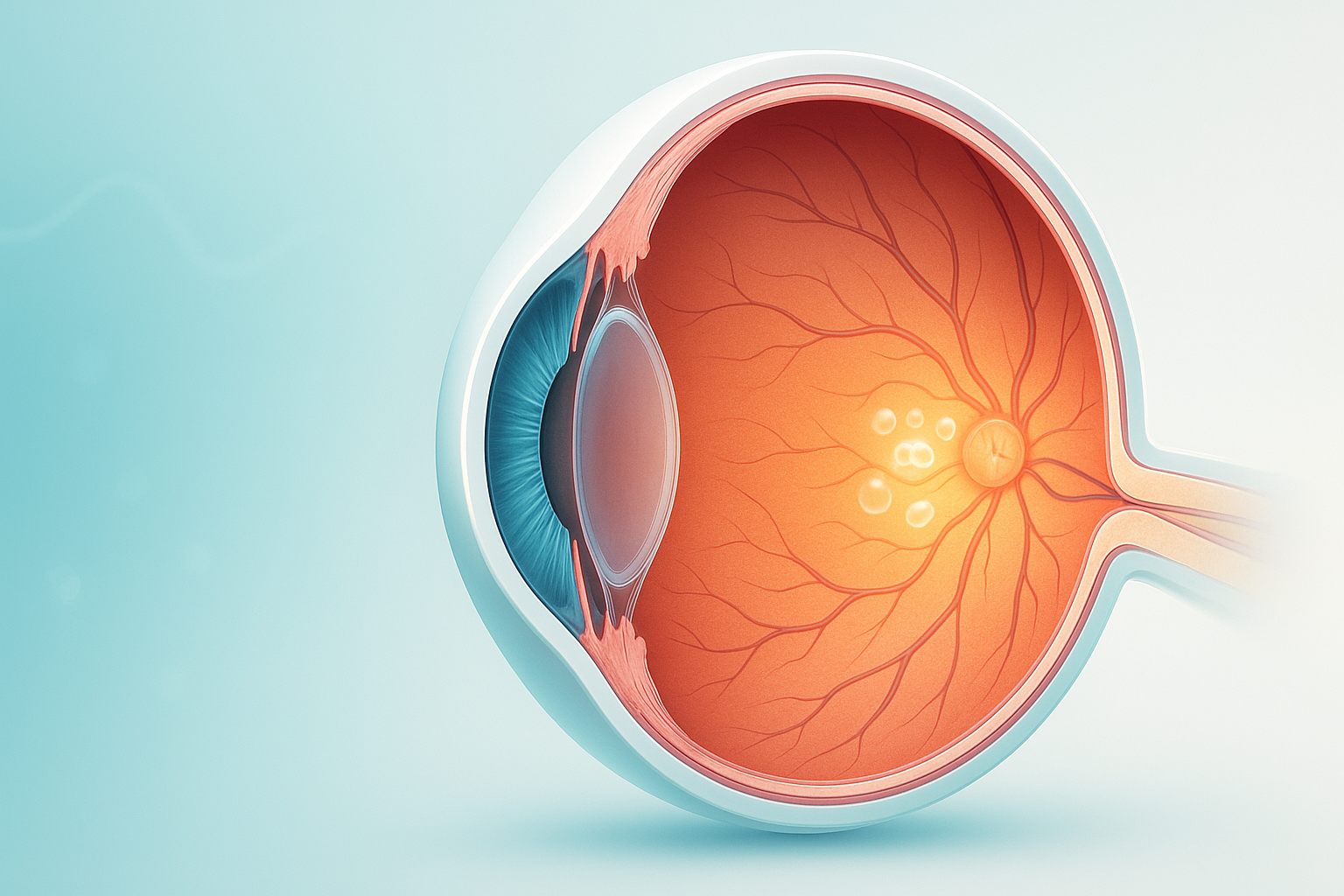
Macular Hole
Causes & Risk Factors
- Age‑related vitreous traction (most common)
- Severe myopia, trauma, prior retinal detachment
Stages (I–IV)
I = impending, II = small full‑thickness, III = larger hole, IV = hole with complete vitreous separation.
Key Symptoms
- Central blur or missing spot
- Lines or letters look broken
Diagnosis
Dilated exam + OCT to measure hole size and stage.
Treatment
- Stage I: observe or enzyme injection (ocriplasmin)
- Stage II–IV: vitrectomy + ILM peel with gas bubble; face‑down positioning 2–5 days (≈ 90–95 % close).
Quick Takeaways
- Pucker = wrinkle on the macula; Hole = break through the macula.
- Both diagnosed swiftly with OCT.
- Early intervention, especially for macular holes, gives the best chance to regain crisp central vision.
- Regular follow‑ups let your retina specialist time surgery before permanent damage sets in.