Eye Condition
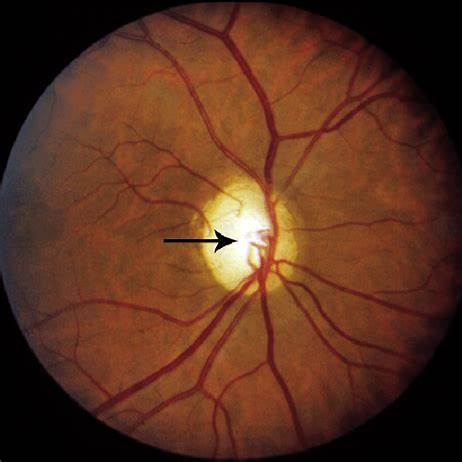
Optic Nerve Atrophy
Optic nerve atrophy limits the optic nerve’s ability to relay visual signals, leading to progressive vision loss.
Explore our treatment options for Optic Nerve Atrophy
What is Optic Nerve Atrophy?
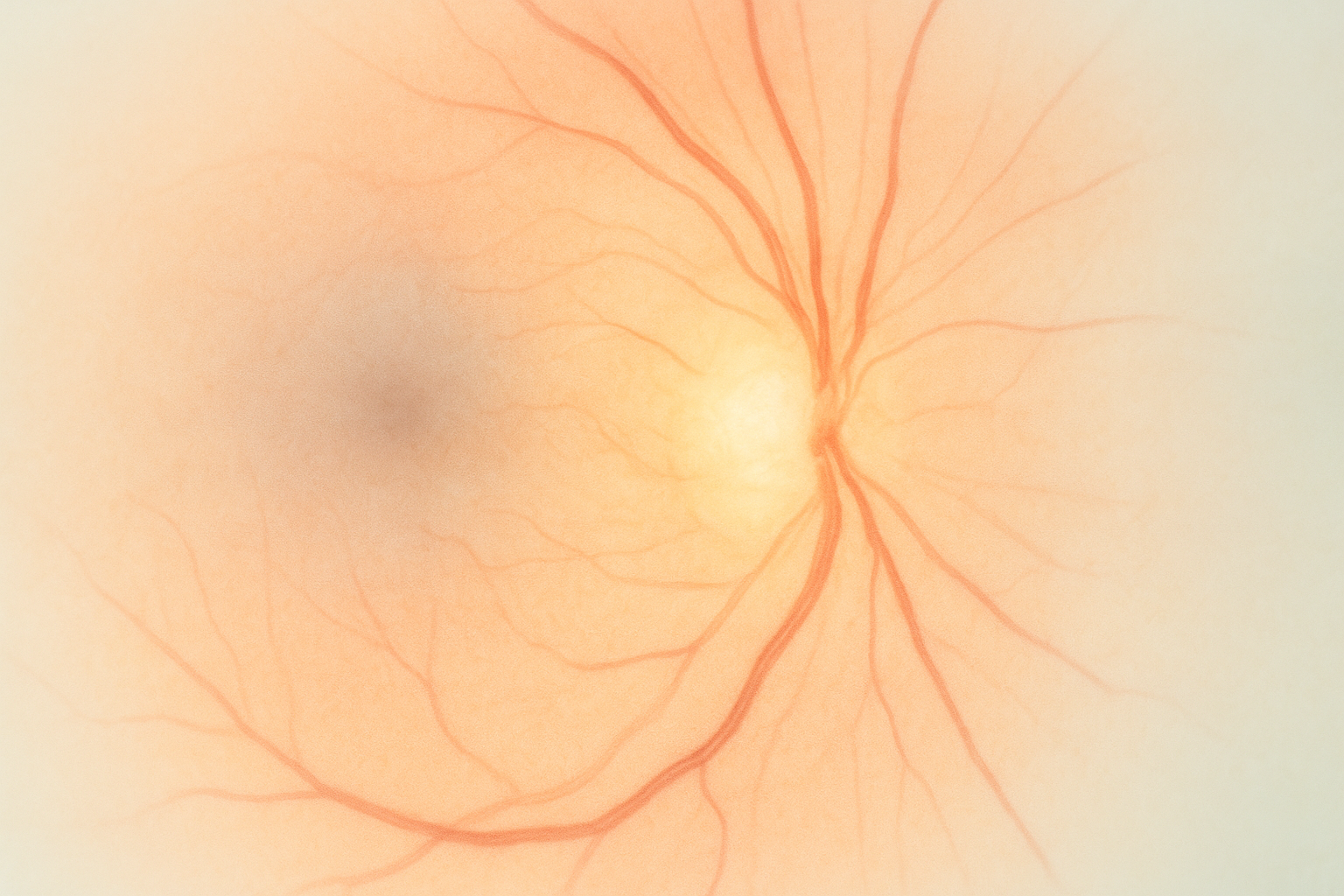
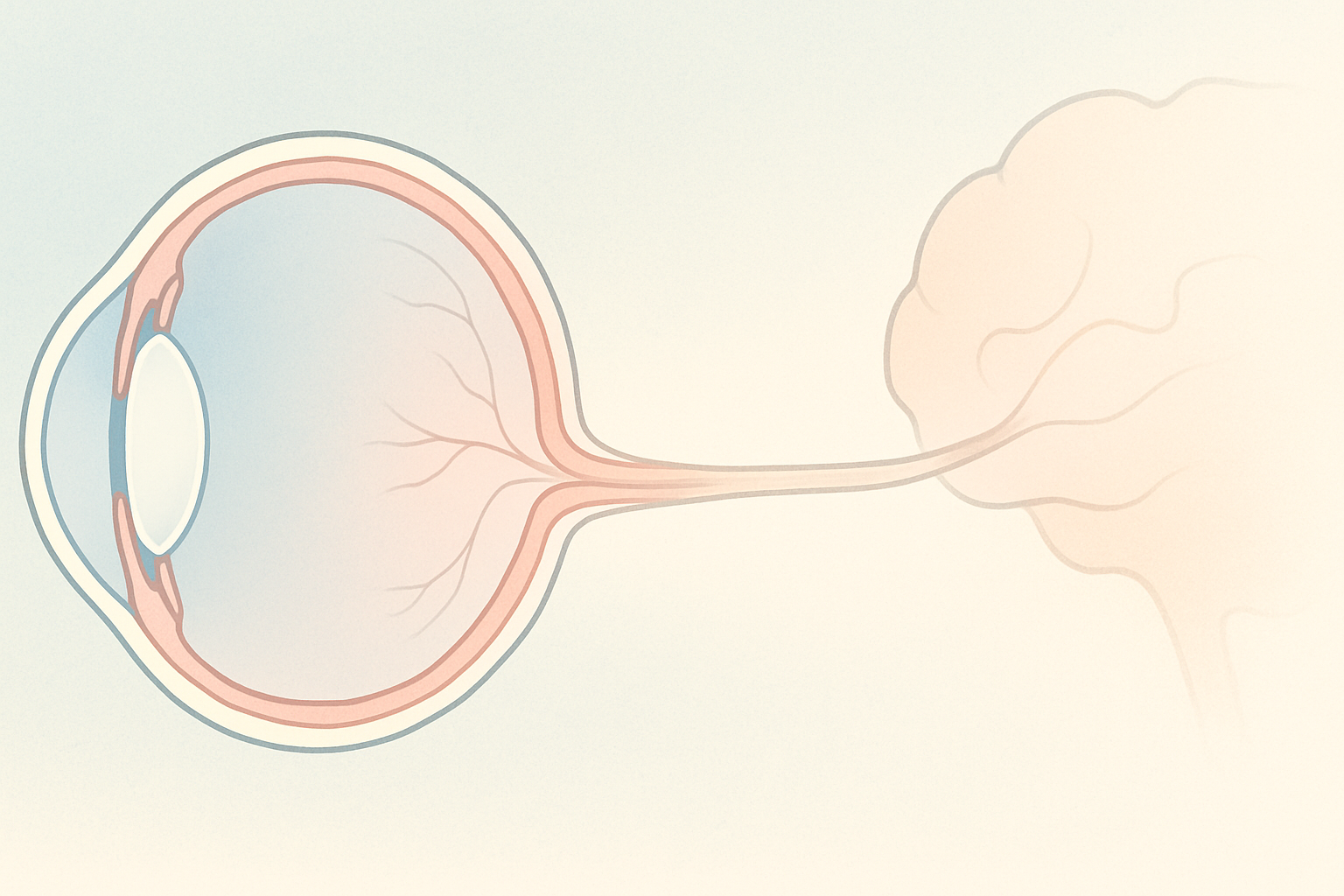
Optic nerve atrophy (ONA), sometimes called optic neuropathy, is the end result of any condition that injures or deprives the optic nerve of oxygen or nutrients. Damage can occur anywhere along the visual pathway from the retina to the lateral geniculate nucleus of the brain. The hallmark is a pale, thinned optic disc that no longer transmits images clearly, resulting in blurred, dim, or missing areas of vision. ONA is not a single disease but a structural change shared by many disorders, from birth defects to adult vascular events.
Key symptoms and early warning signs
- Gradual blurring or dimming of vision in one or both eyes
- Loss of color vibrancy or contrast sensitivity
- Reduced peripheral or central visual field, described as a gray or washed-out area
- Difficulty adapting from light to dark environments
- Urgent sign: sudden vision loss or a curtain-like shadow—which may signal a vascular or inflammatory crisis
Many patients do not notice subtle early changes, so routine eye exams remain critical for detection.
How Optic Nerve Atrophy is diagnosed
Your eye doctor will first view the optic disc through ophthalmoscopy, looking for pallor and thinning. Additional tests include:
- Optical Coherence Tomography (OCT) to measure retinal nerve fiber layer thickness
- Visual field testing to map blind spots and areas of reduced sensitivity
- Visual evoked potential (VEP) to gauge how quickly signals travel to the brain
- Blood work and imaging (MRI/CT) when an inflammatory, infectious, or compressive cause is suspected
These studies help determine whether the damage is stable, worsening, or tied to a treatable underlying disease.
Why it happens: causes and risk factors
Because the optic nerve is metabolically active, it is vulnerable to any event that restricts oxygen, nutrient delivery, or axonal energy production.
- Vascular: ischemic optic neuropathy, giant-cell arteritis, severe hypertension
- Inflammatory: optic neuritis in multiple sclerosis, sarcoidosis, autoimmune uveitis
- Compressive: brain tumors, thyroid eye disease, elevated eye pressure in glaucoma
- Traumatic: head or orbital injuries that shear or compress the nerve
- Toxic and nutritional: chronic alcohol use, tobacco amblyopia, vitamin B12 or folate deficiency, certain antibiotics or antimalarials
- Hereditary and mitochondrial: Leber hereditary optic neuropathy, dominant optic atrophy
Age, systemic inflammation, sleep apnea, poorly controlled diabetes, and high homocysteine can further compromise blood flow and mitochondrial health, raising lifetime risk.
Conventional treatment options
Mainstream ophthalmology focuses on identifying and managing the underlying trigger, reducing eye pressure in glaucoma, high-dose corticosteroids for optic neuritis, urgent steroids for arteritic anterior ischemic optic neuropathy, or surgery to relieve compression. Once the nerve is damaged, there is currently no pharmaceutical that rebuilds optic nerve tissue. Patients are monitored with repeat OCT and visual field tests while low-vision specialists help adapt lighting, contrast, and magnification aids.
Eye Health Institute’s integrative approach
Dr. Andy Rosenfarb’s team views optic nerve health through a broader lens: circulation, mitochondria, neuroinflammation, and neurotrophic support all matter. Our multifaceted program typically combines:
- Micro Acupuncture 48, an evidence-informed acupuncture system that targets ocular microcirculation and has shown functional gains in small pilot studies.
- Pulsed microcurrent stimulation (ACS-3000) around the orbit to enhance ATP production and nerve signaling.
- Targeted nutraceuticals rich in B-complex, alpha-lipoic acid, omega-3s, and antioxidants such as N-acetyl cysteine to combat oxidative stress.
- Mitochondrial support protocols—oral nicotinamide riboside and coenzyme Q10 alongside red-light therapy for energy metabolism.
- Herbal and hydrogen therapies to modulate inflammation and improve endothelial function.
- Lifestyle coaching for glycemic control, anti-inflammatory nutrition, stress regulation, and sleep optimization.
For qualifying patients, we offer one-week in-office “intensive” programs followed by an at-home regimen with loaner microcurrent devices and customized supplement plans. Many individuals report clearer edges, brighter colors, and measurable gains of 2–5 decibels on visual field retesting, though outcomes vary by severity and chronicity.
What patients report and clinical insights
Long-term follow-up suggests that eyes with residual nerve fiber layer above critical threshold respond best, emphasizing the need for early intervention. Patients with ischemic or inflammatory onset often notice faster improvements than those with hereditary forms, but even chronic, stable atrophy can benefit from enhanced contrast and reduced eye fatigue. Our clinicians track progress with OCT, VEP, and subjective questionnaires every three to six months to adjust protocols.

When to seek urgent care
Get urgent eye care right away if you experience sudden vision loss, a curtain-like shadow, painful eye movement with reduced vision, new flashes with multiple floaters, or severe eye pain following injury. These can signal a vascular, inflammatory, or traumatic emergency in the optic nerve and immediate treatment may preserve vision.