Eye Condition
Wet Macular Degeneration
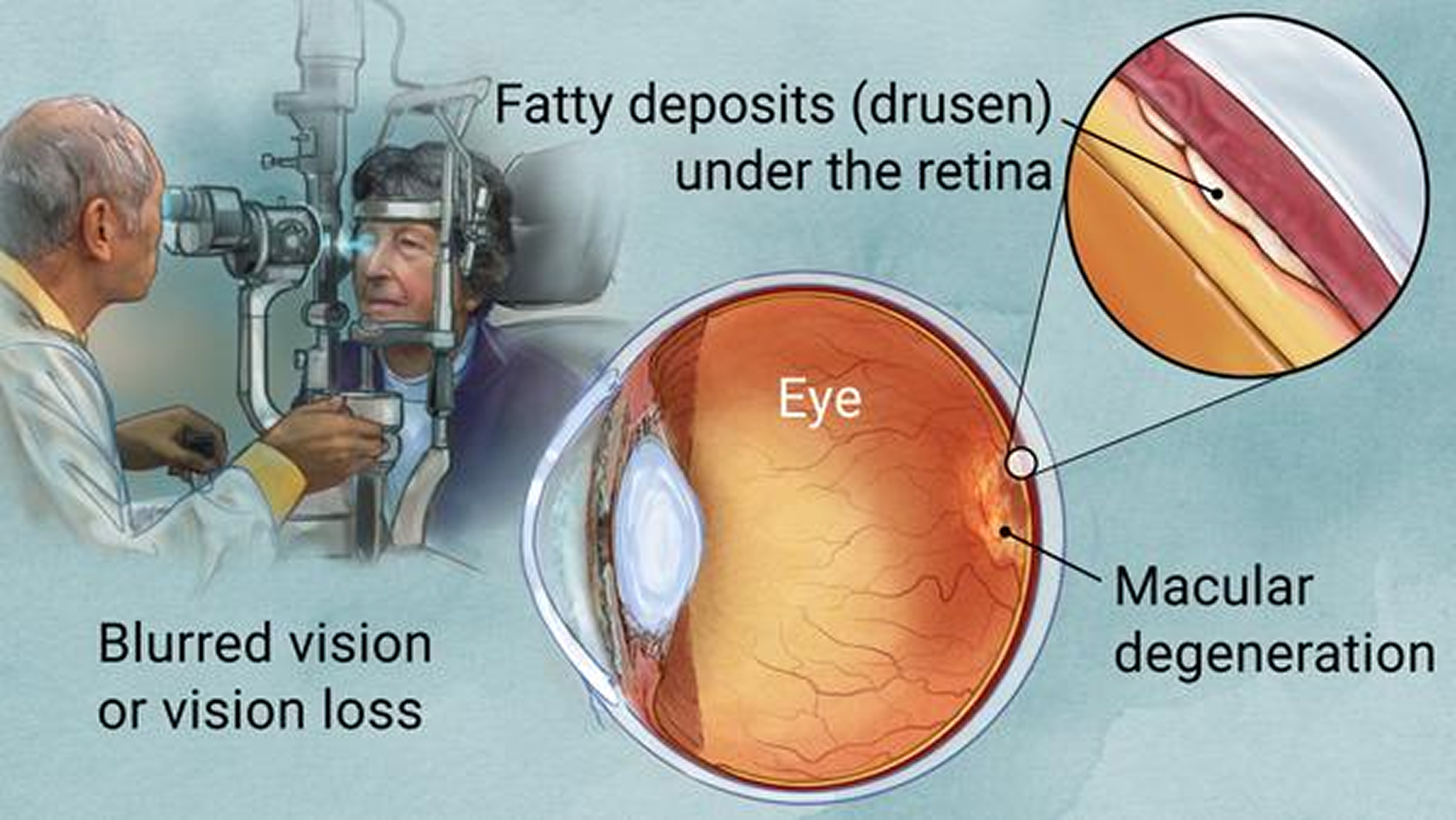
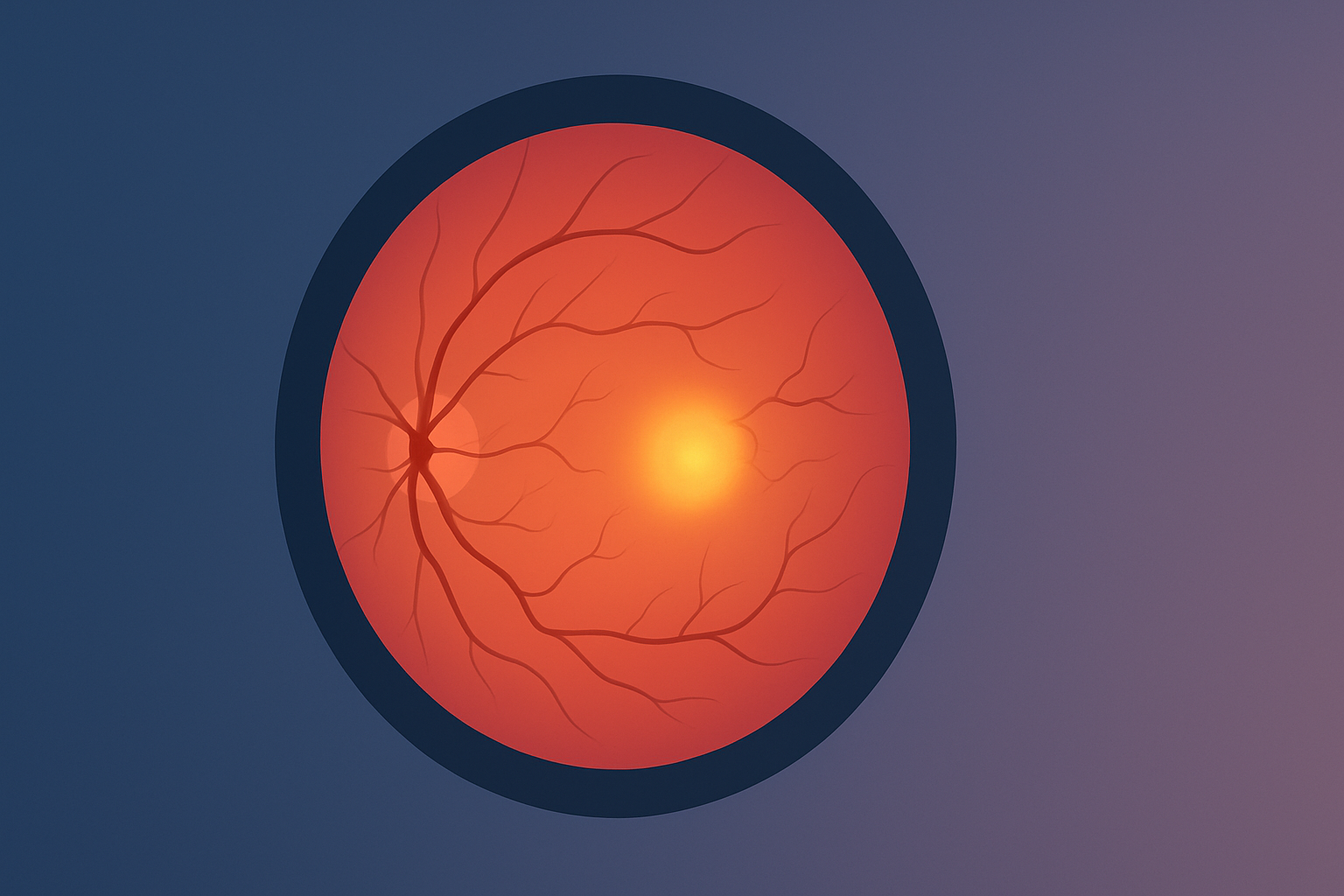
Wet macular degeneration arises when abnormal retinal blood vessels leak beneath the macula, causing rapid distortion and loss of central vision.
Explore our treatment options for Wet Macular Degeneration
What is Wet Macular Degeneration?
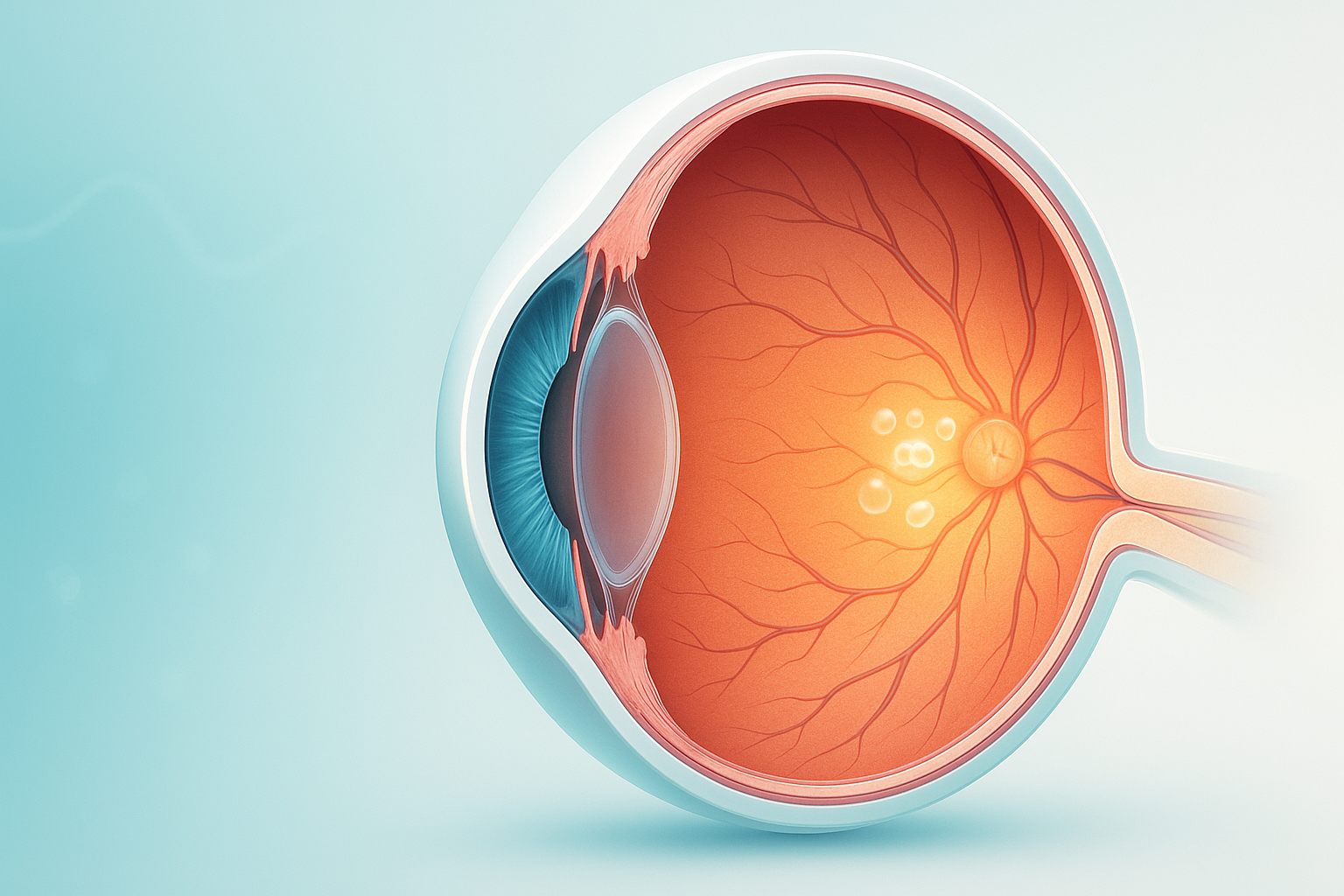
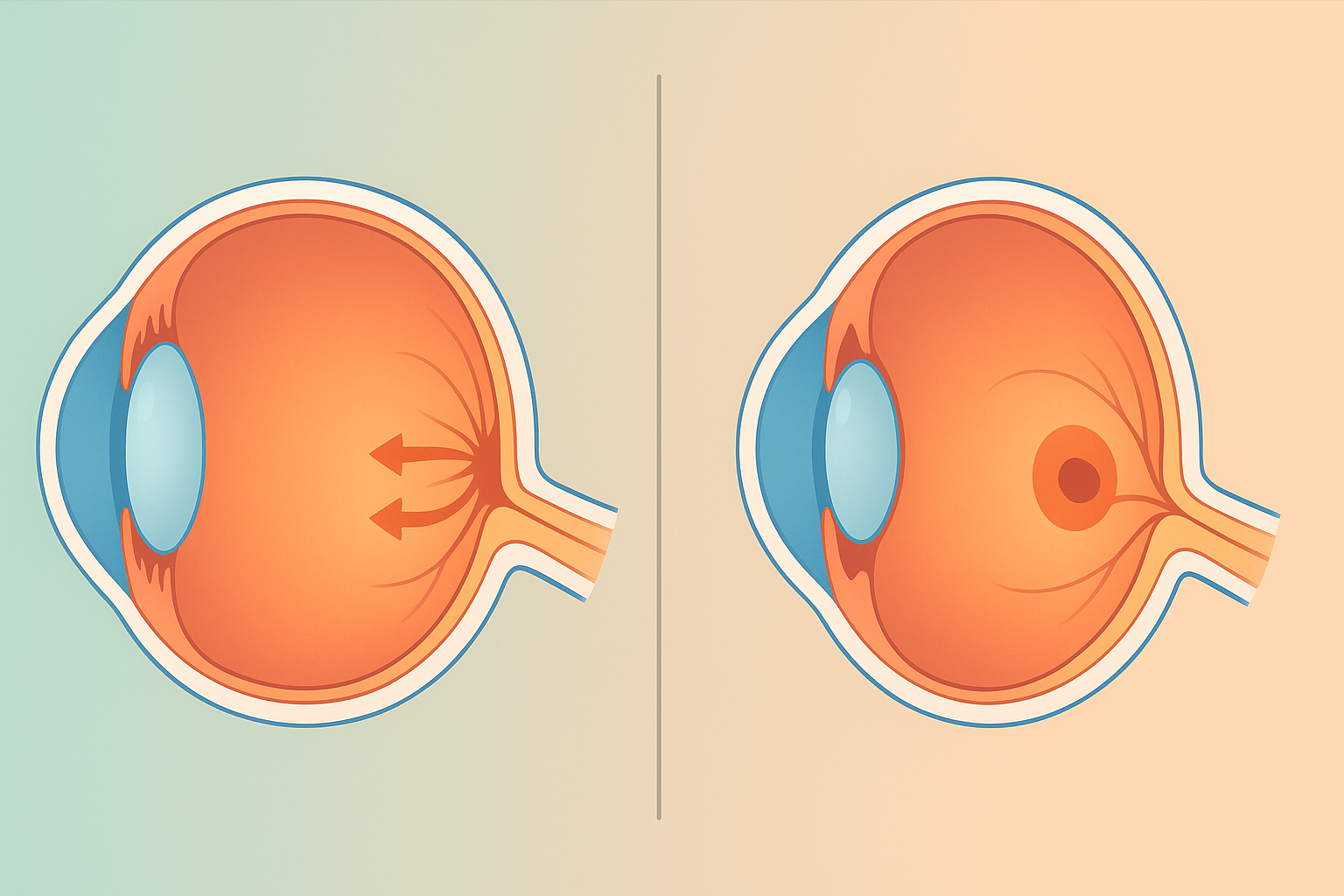
Wet macular degeneration, also known as neovascular age-related macular degeneration (AMD), is a chronic eye condition that leads to the growth of abnormal blood vessels under the retina. These vessels can leak blood and fluid, causing rapid and severe vision loss. Wet AMD primarily affects the central part of the retina, known as the macula, which is crucial for sharp, detailed vision.
Symptoms of Wet Macular Degeneration
- Blurred Vision: Distortion or blurring in the center of your vision.
- Dark or Empty Areas: Presence of dark spots or empty areas in the central vision.
- Visual Distortion: Straight lines appearing wavy or bent.
- Rapid Vision Loss: Sudden and significant loss of central vision.
Causes and Risk Factors
The exact cause of wet macular degeneration is not fully understood, but several risk factors are associated with its development:
- Age: Most common in individuals over 60.
- Genetics: Family history of AMD increases risk.
- Smoking: Smoking significantly raises the risk of developing AMD.
- Obesity: Higher body mass index (BMI) is linked to an increased risk.
- Cardiovascular Disease: Conditions affecting the heart and blood vessels may contribute to AMD.
Diagnosis
Early detection is critical for managing wet macular degeneration and preserving vision. Our clinic offers comprehensive diagnostic services, including:
- Ophthalmic Examination: Detailed eye examination using slit-lamp biomicroscopy.
- Optical Coherence Tomography (OCT): High-resolution imaging to detect fluid or blood under the retina.
- Fluorescein Angiography: Imaging test to visualize blood vessels in the retina.
- Amsler Grid Test: Simple test to detect visual distortions.