Eye Condition
Fuchs Dystrophy
Fuchs corneal dystrophy causes gradual corneal cell loss that can swell and cloud your cornea.
Explore our treatment options for Fuchs Dystrophy
What is Fuchs Dystrophy?
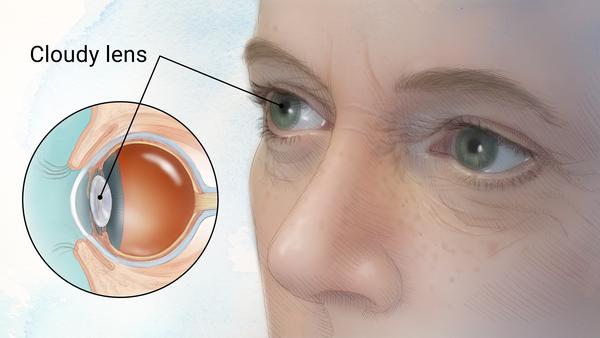
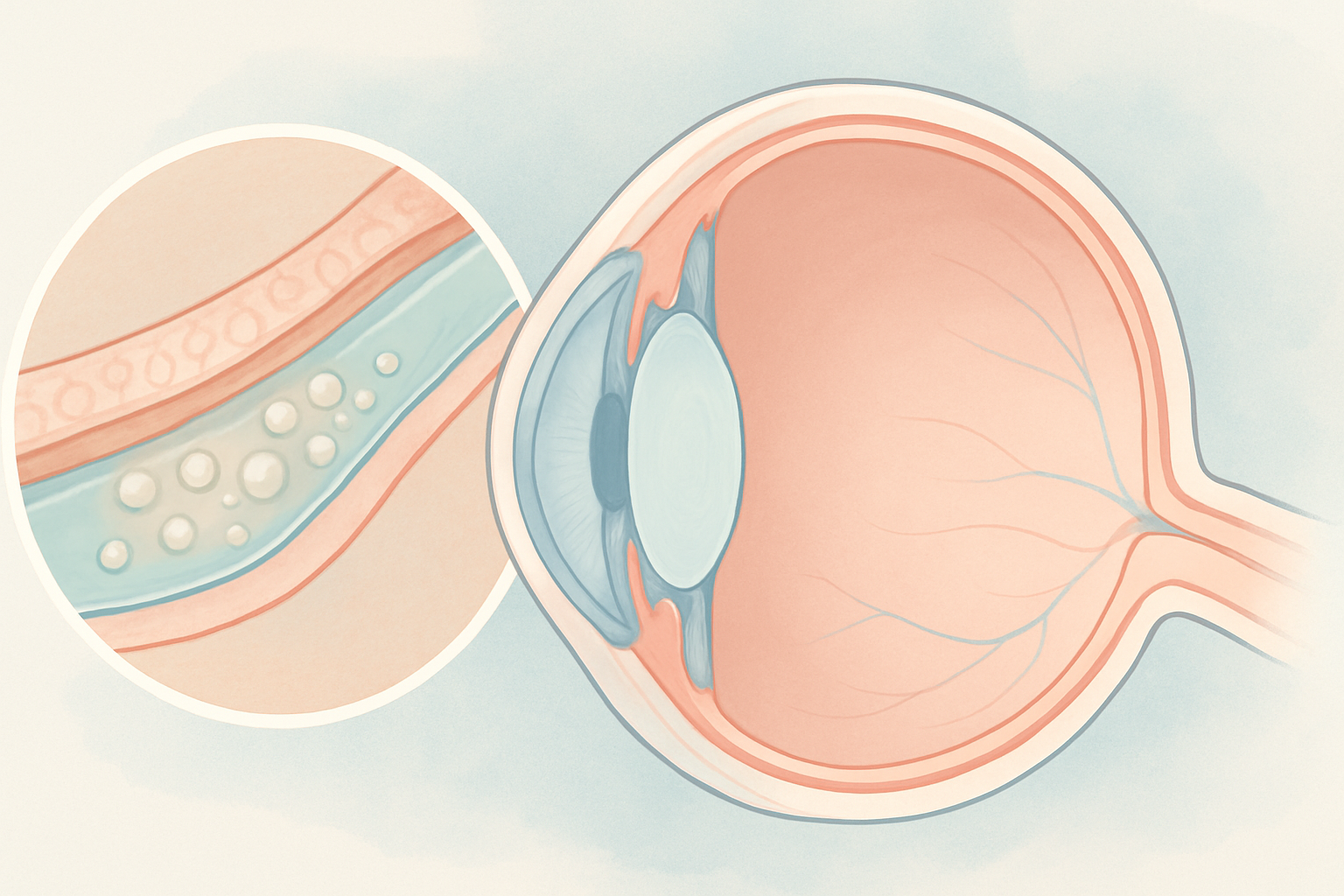
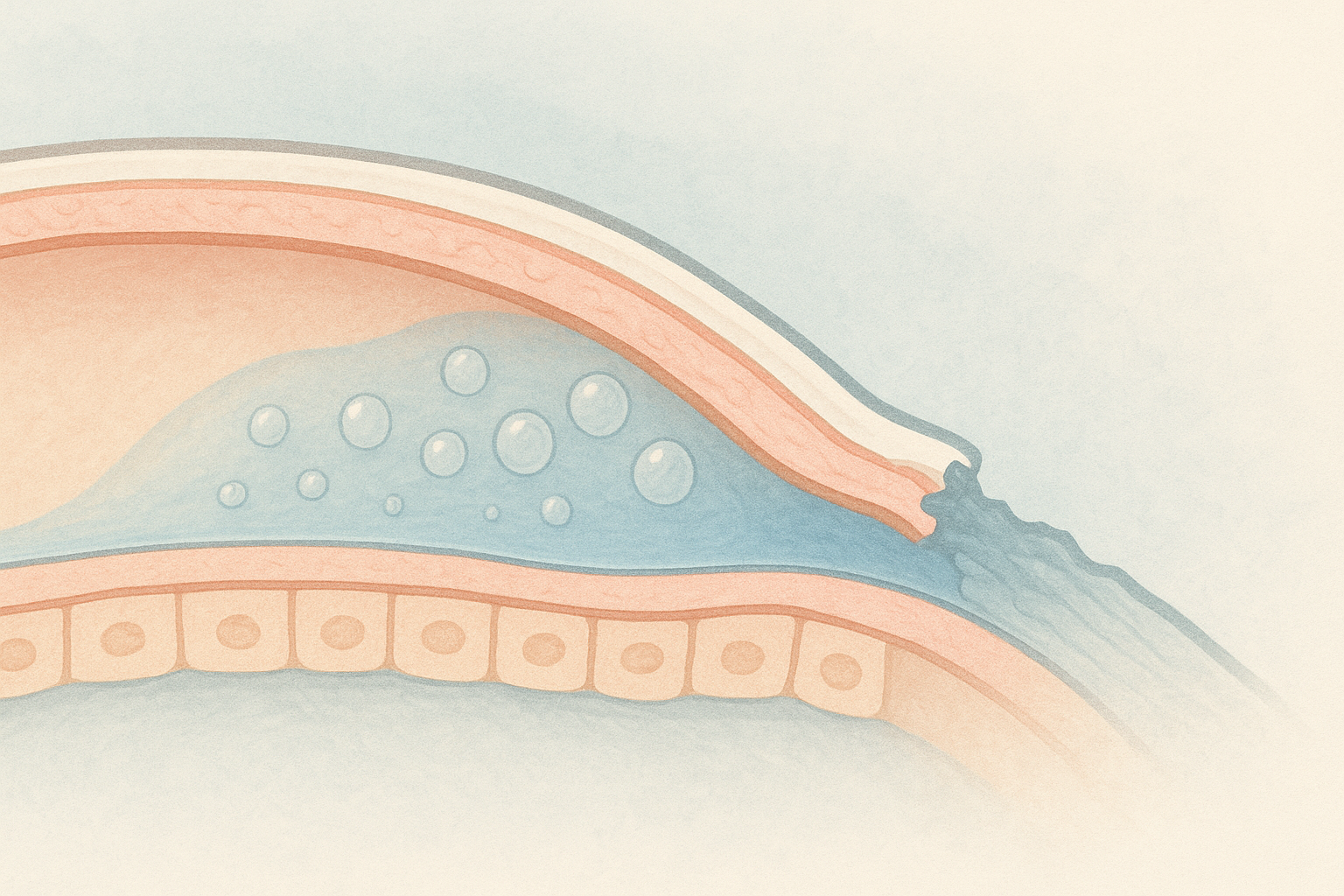
Fuchs dystrophy (Fuchs endothelial corneal dystrophy) is a slowly progressive disease in which the innermost layer of the cornea (the endothelial cells) degenerates. These cells normally pump excess fluid out of the cornea to keep it thin and transparent. When enough cells are lost, fluid builds up, the cornea thickens, and tiny blisters (bullae) can form on the surface. Vision becomes hazy, especially in the morning, and the eye may feel gritty or light-sensitive. The condition generally affects both eyes and advances over decades, although each eye can progress at a different pace.
Key symptoms and early warning signs
- Blurred or foggy vision on waking that clears gradually
- Glare and halos around lights, especially at night
- Sudden sharp pain if surface blisters rupture
- Sandy or gritty eye sensation
- Heightened light sensitivity or difficulty driving in low light
- Progressive decline in best-corrected vision over years
How Fuchs Dystrophy is diagnosed
Eye doctors combine several tests to confirm and stage Fuchs dystrophy:
| Test | What it shows |
|---|---|
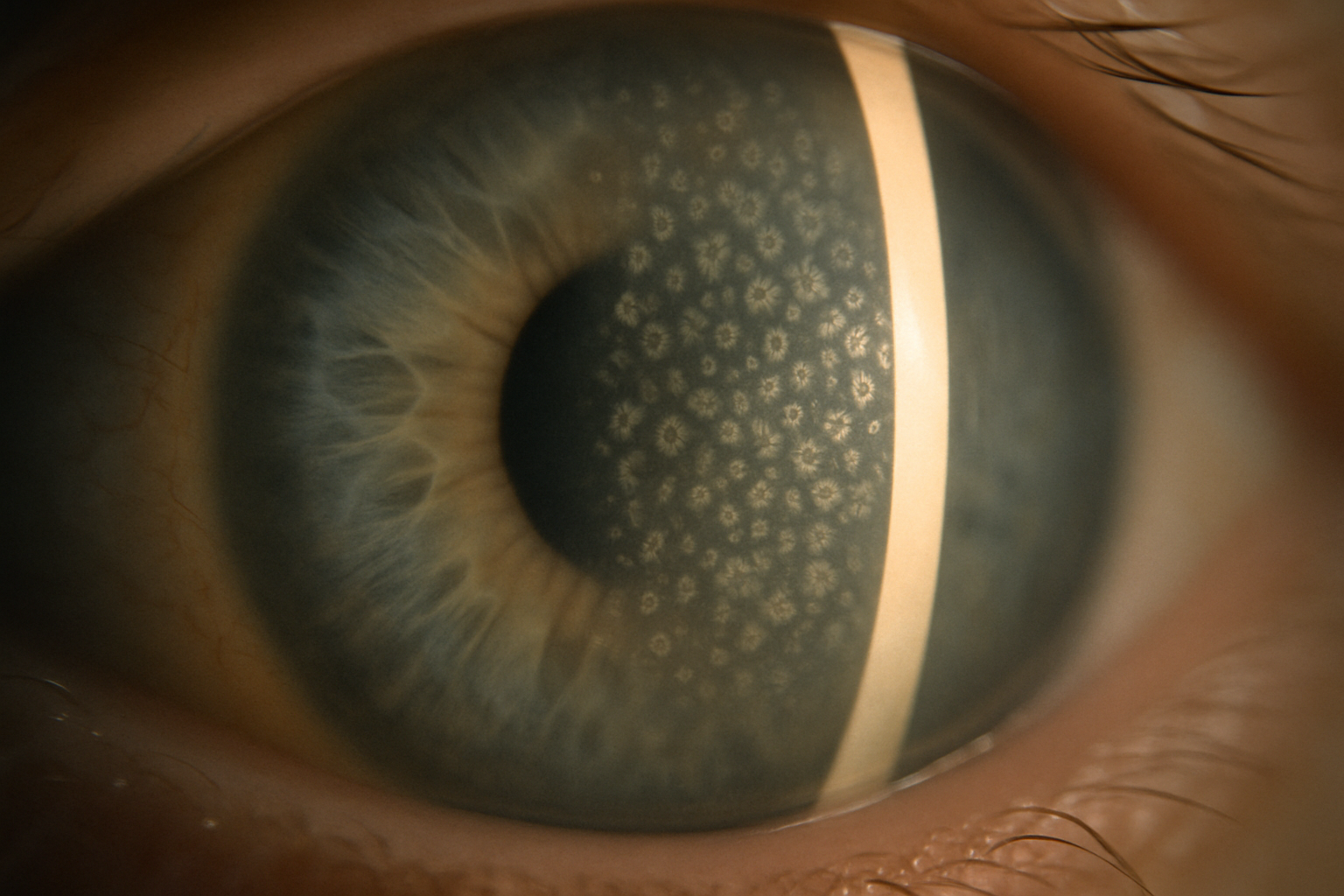
| Slit-lamp exam | Tiny bumps called guttae on the back surface of the cornea |
| Corneal pachymetry | Measures thickness to track swelling |
| Specular microscopy or confocal imaging | Counts living endothelial cells |
| Optical coherence tomography (OCT) | Cross-sectional view of corneal layers |
Early diagnosis helps you and your doctor plan lifestyle adjustments and, if needed, time surgical care such as endothelial keratoplasty or combined cataract surgery and corneal transplant.
Why it happens: causes and risk factors
Fuchs dystrophy is usually inherited in an autosomal dominant pattern, meaning a child has a 50 percent chance of developing it if one parent is affected. Researchers have linked it to mutations in the TCF4 gene that alter endothelial cell metabolism. Other risk factors include:
- Female sex: women are two to four times more likely to develop symptomatic disease
- Family history of Fuchs dystrophy
- Age over 50 for noticeable vision changes (subclinical changes may start in the 30s or 40s)
- History of eye surgery or trauma that reduces endothelial cell reserve
- Elevated oxidative stress and chronic inflammation
While the genetic component cannot be changed, supporting corneal metabolism and reducing oxidative damage may help slow functional decline.
Conventional treatment options
Mainstream care focuses on managing corneal swelling and, when necessary, replacing the failing cell layer:
- Hypertonic saline 5 % drops or ointment draw out corneal fluid and reduce morning blur.
- Drying the cornea with a handheld hair dryer at arm’s length can evaporate surface water.
- Bandage contact lenses ease pain from ruptured blisters.
- Endothelial keratoplasty (DSAEK or DMEK) selectively replaces the diseased layer with healthy donor tissue and is now preferred over full-thickness transplants.
- Combined cataract and DMEK surgery is common because many patients develop lens clouding as corneal clarity declines, making a single-stage procedure more efficient.
- Rho-kinase inhibitor eye drops are undergoing study to stimulate cell healing.
Recovery from surgery is usually quick, yet grafts require lifelong monitoring. Many patients look for supportive therapies to stay comfortable and delay or avoid surgery when possible.
Eye Health Institute’s integrative approach
Dr. Andy Rosenfarb and the Eye Health Institute team combine conventional ophthalmology with evidence-guided natural medicine to address metabolic stress on corneal cells. While no alternative therapy can replace lost endothelium, supporting mitochondrial function and tear film stability may help patients stay comfortable and buy time before surgery.
Our typical program may include:
- Micro Acupuncture 48 to encourage ocular blood flow and reduce oxidative stress signals that damage endothelial pumps.
- Electroacupuncture and microcurrent therapy (ACS-3000) applied around the eyes to stimulate corneal wound healing pathways and calm pain from ruptured bullae.
- Targeted herbal and nutritional supplementation such as astaxanthin, vitamin C, N-acetylcysteine, and omega-3 fatty acids to support glutathione recycling and cell membrane integrity.
- Hydrogen inhalation therapy aimed at neutralizing excess reactive oxygen species in anterior chamber fluid.
- Moisture chamber goggles and environment coaching to maintain a stable tear film, reduce surface blistering, and improve morning vision.
- Stress and lifestyle counseling on sleep posture, indoor humidity, and blue-light management to reduce overnight edema and glare.
- Intensive on-site programs or at-home maintenance kits let you choose the depth of care that fits your schedule.
Our clinicians coordinate closely with your corneal specialist to track pachymetry and cell counts. If surgery becomes the clear next step, pre- and post-operative acupuncture may improve comfort and reduce inflammation for smoother healing. Patients often report steadier vision, less morning fog, and greater confidence in daily tasks while under integrative care.
What patients report / clinical insights
Many people arrive at EHI worried about the unpredictability of their vision from one day to the next. After several weeks on an individualized integrative plan they often describe:
- Fewer episodes of stabbing pain from ruptured bullae
- Shorter “foggy” periods after waking
- Better tolerance of bright lights and screens
- More mental ease knowing active steps are in place to support eye health
These subjective improvements can translate into a higher quality of life while medical monitoring continues.
When to seek urgent care
Get urgent eye care if you notice sudden vision loss, a curtain-like shadow, many new floaters with flashes, severe eye pain, or direct eye trauma. With Fuchs dystrophy specifically, seek same-day care if:
- Vision stays cloudy all day rather than clearing after waking
- Sharp surface pain becomes constant or is accompanied by redness
- You develop swelling that stops you from driving or working safely
Prompt evaluation helps prevent infection, scarring, or a painful rise in eye pressure.