Eye Condition
Vitreous Detachment
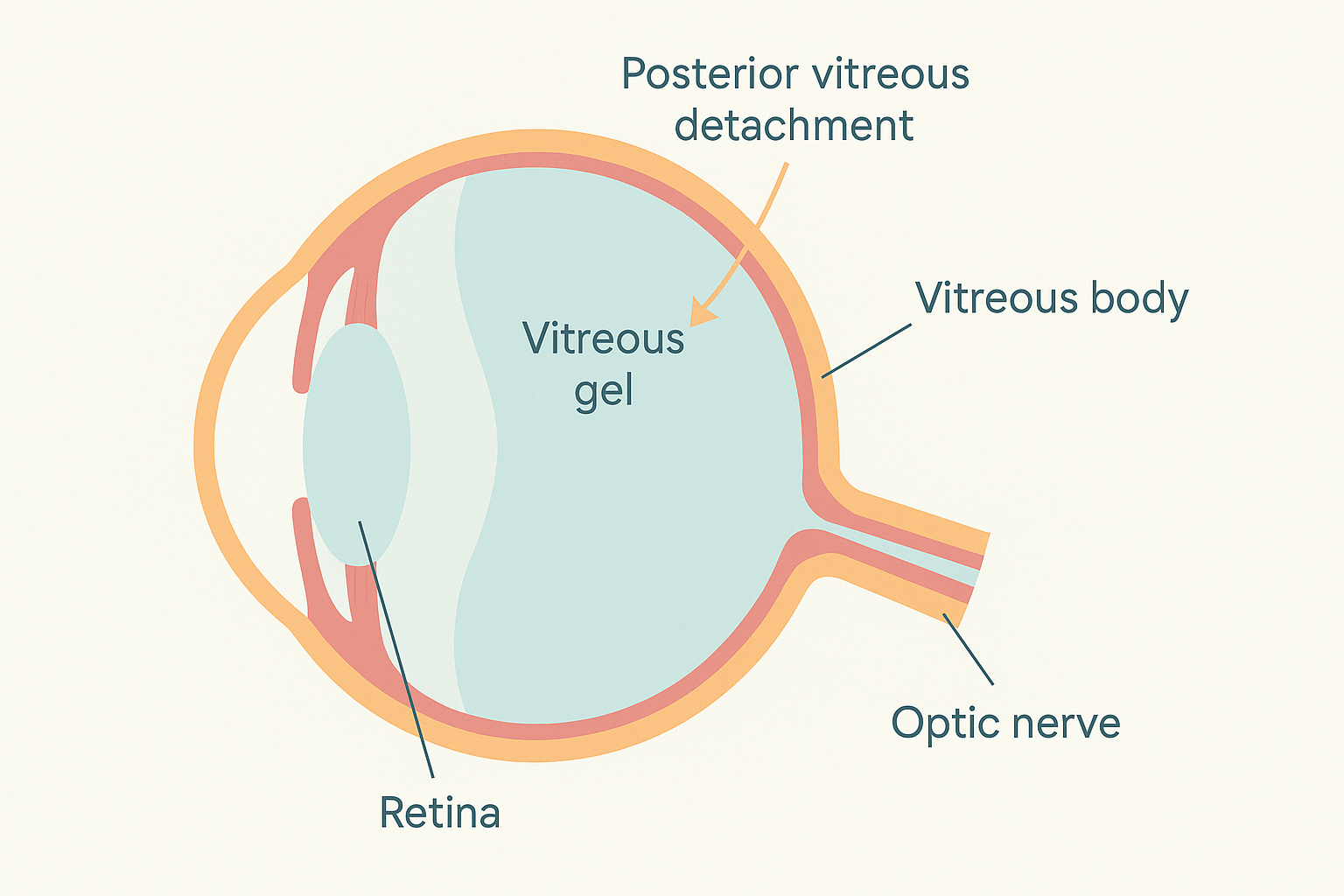
Vitreous detachment is a common eye condition that occurs when the vitreous gel, the clear jelly-like substance in the eye, separates from the retina.

Explore our treatment options for Vitreous Detachment
What is Vitreous Detachment?
The vitreous is a clear, jelly-like substance that fills the large central cavity of the eye and helps it keep its round shape. With time, this gel naturally shrinks, liquefies, and pulls away from the retina, the light-sensing tissue lining the back wall of the eye. When that separation becomes complete the process is called posterior vitreous detachment, or simply vitreous detachment.
Most people experience it after age 50. In many cases the event is benign: vision stabilizes and no treatment is needed. However, in roughly 10 percent of eyes the pulling force can tug hard enough to tear the fragile retina, setting the stage for a potential retinal detachment. Because that sight-threatening complication cannot be felt, recognizing early warning signs is essential.
Key symptoms and early warning signs
- Floaters – moving specks, strings, or cobwebs that drift with eye movement
- Flashes of light – brief arcs or lightning-like streaks in side vision
- New haziness or blurring that does not clear with blinking
- A sudden shower of many tiny dots or a large floater (possible retinal tear)
- Peripheral shadow or curtain advancing across vision – an urgent red flag
Symptoms often appear suddenly and are more obvious against bright backgrounds such as a clear sky or computer screen. Mild floaters alone are common, but a rapid increase combined with repeated flashes deserves prompt examination within 24 hours.
How Vitreous Detachment is diagnosed
Your eye doctor will start with a detailed history of symptoms and then perform tests to look for retinal damage:
- Dilated slit-lamp biomicroscopy – the classic chair-side examination with bright light and lenses lets the doctor inspect both vitreous and retina.
- Indirect ophthalmoscopy with scleral depression – gentle pressure on the eyelids gives a panoramic view of the far edge of the retina where tears often hide.
- Optical Coherence Tomography (OCT) – high-resolution infrared imaging reveals subtle traction or microscopic splits between layers.
- B-scan ultrasound – helpful when the view is clouded by dense floaters or cataract.
At Eye Health Institute we combine these tests so patients leave knowing whether the retina is intact or needs emergency laser sealing.
Why it happens: causes and risk factors
Aging is the primary driver. Collagen fibers that once formed a firm three-dimensional network uncoil with time, causing pockets of liquid to develop inside the vitreous. Eventually that watery pocket coalesces, the remaining strands collapse, and the gel detaches. Factors that promote earlier or stronger traction include:
- Age over 50 – prevalence rises sharply each decade.
- Myopia (nearsightedness) – longer eyes stretch the gel, increasing stress.
- Previous eye surgery such as cataract extraction or LASIK.
- Eye trauma – even mild blows can trigger abrupt liquefaction.
- Inflammation from uveitis or autoimmune disease.
- Family history of retinal tears or detachment.
- Systemic connective-tissue disorders that weaken collagen.
Smoking, poorly controlled blood sugar, and high homocysteine may degrade ocular collagen as well, though the evidence is still emerging.
Conventional treatment options
There is no medication that can stop or reverse vitreous detachment; the process is mechanical and usually self-limited. Standard medical care focuses on monitoring for retinal breaks:
- Immediate dilated exam at symptom onset
- Follow-up exam within 4–6 weeks even if symptoms fade
- Early laser retinopexy or cryotherapy to seal any tear before fluid passes through it
- Vitrectomy surgery only if dense floaters seriously impair daily tasks or if persistent traction threatens macular vision
The majority of patients require no intervention beyond reassurance and scheduled check-ups.
Eye Health Institute’s integrative approach
Dr. Andy Rosenfarb’s team looks beyond simply waiting for the gel to settle. We aim to support the health and resilience of the retina during and after detachment:
- Micro Acupuncture 48 – targeted points around the orbit may enhance retinal blood flow and nerve metabolism, encouraging faster adaptation.
- Frequency-specific microcurrent (ACS-3000) – gentle, pulsed electric current applied through closed eyelids can calm inflammation and promote collagen remodeling.
- Herbal and nutritional support – formulas rich in collagen peptides, vitamin C, proanthocyanidins, and taurine nourish the vitreous while antioxidants safeguard retinal photoreceptors.
- Mitochondrial rescue with molecular hydrogen – hydrogen-infused water or eye baths may reduce oxidative stress spikes that accompany traction.
- Lifestyle coaching – we address blood sugar balance, posture ergonomics, and safe exercise guidelines to minimize further tugging.
- Intensive in-office programs or at-home protocols – patients choose the schedule that fits their life yet still benefit from personalized care.
Our goal is twofold: lower the chance of a retinal tear and help your visual system recalibrate to the new optical environment so floaters become less intrusive.
What patients report / clinical insights
Many EHI patients arrive anxious after a sudden burst of floaters and flashes. Within days of starting supportive therapies they often describe:
- Faster fading of bright arcs
- Floaters that sink below the central line of sight
- Less eye strain when reading or working at a screen
- Peace of mind from understanding how to self-monitor
Long-term follow-up suggests that patients who embrace the integrative program maintain stable retinal health and rarely progress to detachment, matching favorable outcomes reported in conventional ophthalmology while adding improved quality of life. Individual results vary, but empowerment through education and proactive care is a constant.

When to seek urgent care
Get urgent eye care today if you experience any of the following:
- A sudden shower of new floaters like pepper or gnats
- Repeated, bright flashes of light that persist longer than a day
- A gray curtain, veil, or shadow sliding across any part of your vision
- Sudden loss of side vision, even if central vision seems clear
- Severe eye pain or blunt trauma to the eye
These signs may indicate a retinal tear or detachment that requires same-day laser treatment or surgery to save vision.