Eye Condition
Retinitis Pigmentosa
Retinitis pigmentosa is an inherited retinal disorder that gradually destroys photoreceptor cells, leading to night blindness and progressive tunnel vision.
Explore our treatment options for Retinitis Pigmentosa
Retinitis Pigmentosa (RP) - Overview
Retinitis Pigmentosa (RP) is an umbrella term covering more than 90 genetic disorders that slowly destroy the retina's photoreceptors. Each subtype is a little different, yet they all share one hallmark: gradual loss of vision that almost always begins with night-blindness and, if untreated, can end in severe tunnel vision or total blindness. RP is rare, about 1 in 4,000 people in the United States, but it is the most common inherited retinal dystrophy worldwide.
Fast Facts
- Primary target: Rod cells (night & peripheral vision); later cones (central vision)
- Common first symptom: Night‑blindness (nyctalopia)
- Usual progression: Peripheral → mid‑peripheral → central ("tunnel vision")
- Inheritance patterns: Autosomal dominant, recessive, X‑linked, and sporadic
- FDA‑approved gene therapy: Luxturna (RPE65‑specific; under 1% of RP cases)
- Clinical‑trial pipeline: CRISPR prime‑editing, optogenetic MCO‑010, neuro‑protective eye drops
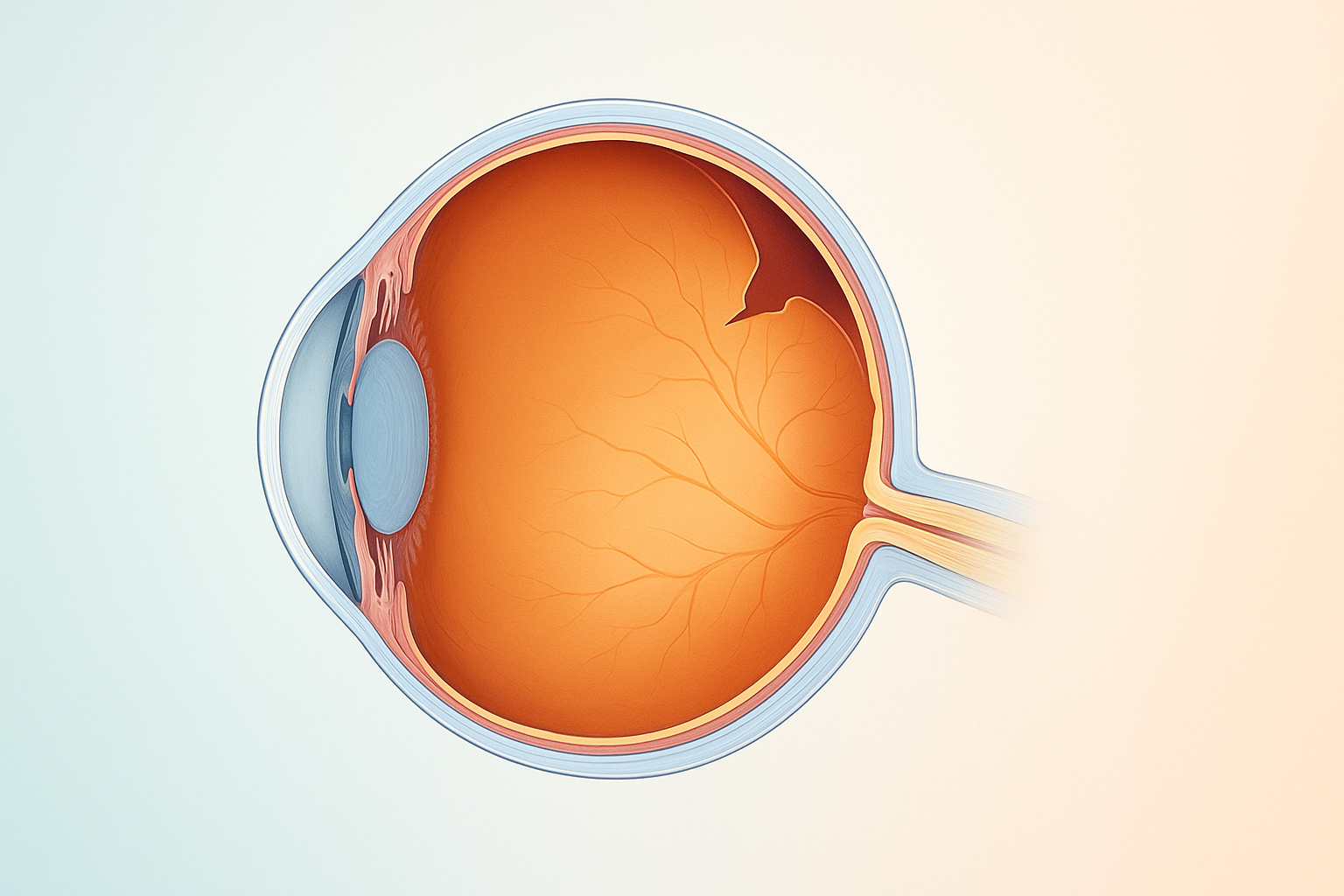
What Happens in Retinitis Pigmentosa?
Mutations disrupt the proteins that keep photoreceptors healthy. Rods, the cells that let you see at night, die first. Over time, cones in the macula are also damaged, narrowing usable vision until the world looks like you're peering through a paper-towel tube.
It's usually okay in the central vision, usually pretty okay in the far periphery, and as RP progresses it moves inward … to the point where we just have a pinhole left.
Key Symptoms & Red Flags
- Night‑blindness: trouble in dim restaurants, at dusk, or in movie theaters
- Flash‑like photopsias or “visual snow” indicating retinal irritation
- Loss of contrast (reds/greens, browns/purples look muddy)
- Shrinking side vision that evolves into a tunnel‑like view
- Slow adaptation when moving from bright sunlight to indoors
- Complications
- Cystoid Macular Edema (CME)
- Early cataracts
- Hearing loss in Usher Syndrome
Emergency: A sudden shower of floaters, flashes, or a dark “curtain” over your sight can signal a retinal tear or detachment—call your retina specialist within 24 h.
How RP Is Diagnosed
| Test | What it reveals |
|---|---|
| Dilated fundus exam | Bone‑spicule pigment & narrowed vessels |
| Optical Coherence Tomography (OCT) | Thinning photoreceptor layer, CME pockets |
| Visual field (Goldmann / Humphrey) | Maps tunnel vision over time |
| Electro‑retinography (ERG) | Electrical response of rods & cones |
| Comprehensive gene panel | Identifies the causative mutation ∼70 % of the time |
Why Drug Development Is Hard
More than 3,000 mutations can trigger RP, so a one‑gene/one‑drug model is slow. Even when a therapy works, Luxturna corrects RPE65, the vast majority of patients remain untreated. Gene‑agnostic approaches (e.g. CRISPR base‑editing, optogenetics, and artificial-retina chips are in early trials, but everyday care is still the frontline defense.
Proven Ways to Slow Progression Now
Anti‑inflammatory lifestyle
- Mediterranean or low‑glycemic diet
- Eliminate food allergies (IgG blood test)
- Adequate sleep & daily stress relief (breath‑work, yoga, cardio)
Core retina nutrients
- Vitamin A palmitate (under medical supervision)
- Omega‑3 DHA — 1‑2 g/day
- Carotenoids — lutein, zeaxanthin, meso‑zeaxanthin, astaxanthin
- Full‑spectrum CBD for neuro‑inflammation
Targeted medical care
- Laser or cryopexy to seal peripheral tears
- Carbonic‑anhydrase inhibitors for CME
- Hyperbaric oxygen or low‑level laser therapy (LLLT) to boost retinal oxygenation
Low‑vision rehabilitation
- Field‑expanding prism glasses, reverse telescopes
- Orientation & mobility training; white‑cane skills
- Screen‑reader apps, smart lighting at home
Lifestyle Checklist
| ✅ Do | 🚫 Avoid |
|---|---|
| 30 min brisk walking or cycling daily | Smoking or vaping |
| 100 % UV‑A/UV‑B sunglasses + blue‑block lenses | Excess alcohol & refined sugar |
| Leafy greens, oily fish, nuts, seeds | Ultra‑processed snacks & sodas |
| Annual dilated‑eye exam (6 mo if symptomatic) | Skipping follow‑ups |
Bottom Line
RP isn't hopeless. A mix of regular monitoring, smart lifestyle changes, and emerging therapies can often preserve useful vision for decades, and may even recover a little of what's been lost. If you have further questions, drop a comment below or book a tele-consult with the Eye Health Institute team.
Your vision is our mission.
Learn More
Explore our comprehensive guides on retinitis pigmentosa:
- Causes of Retinitis Pigmentosa
- Is Retinitis Pigmentosa an Autoimmune Disease?
- Epigenetics and Retinitis Pigmentosa
- Retinitis Pigmentosa Symptoms
- Cystoid Macular Edema in RP
- Conditions Related to Retinitis Pigmentosa
- Usher Syndrome and Retinitis Pigmentosa
- Stargardt's Disease vs Retinitis Pigmentosa
- Functional Medicine for Retinitis Pigmentosa
- Prevention Strategies for Retinitis Pigmentosa
- Best Supplements for Retinitis Pigmentosa
- Diet and Lifestyle for Retinitis Pigmentosa
- Updated Retinitis Pigmentosa Treatment Options 2026