Eye Condition
Eye Floaters
Eye floaters are tiny drifting shapes caused by age-related changes in the eye’s vitreous gel, and while usually harmless they can sometimes signal retinal danger.
Explore our treatment options for Eye Floaters
What Are Eye Floaters?
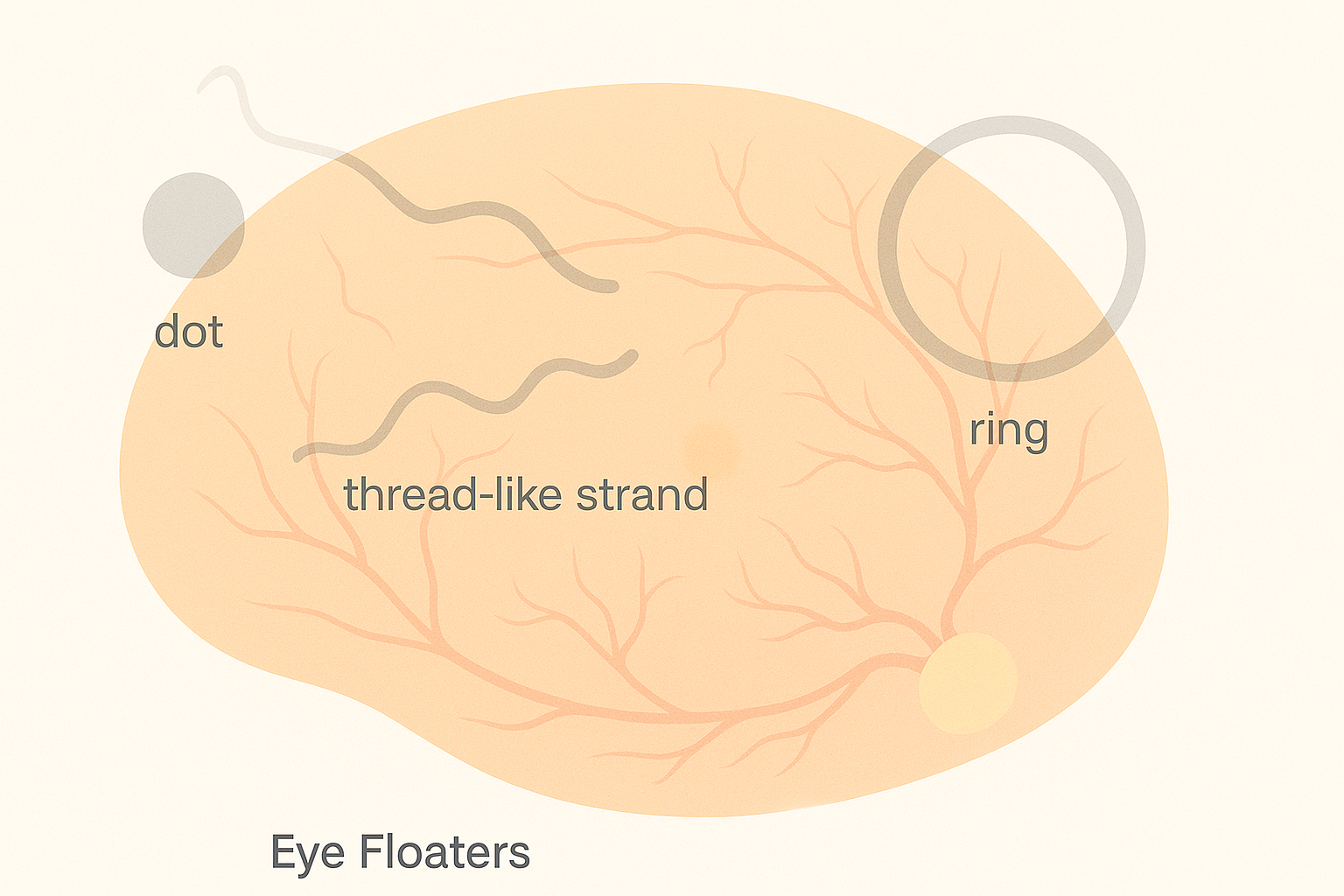
Eye floaters, medically called myodesopsia, are the small gray or black specks, strings, or cobweb-like shapes that move across your field of vision. They appear when condensed collagen fibers or microscopic clumps of protein cast shadows onto the light-sensitive retina. Most floaters drift as your eyes move and seem to dart away when you try to look at them directly, settling when your gaze is still.
Key symptoms and early warning signs
- Specks, threads, rings, or clouds that move as your eyes move
- Shapes that are most noticeable against bright backgrounds such as a blue sky or white screen
- Gradual increase in number over years is typical with aging
- Urgent sign: a sudden shower of new floaters, flashes of light, or a gray curtain in side vision can indicate a retinal tear or detachment
How Eye Floaters are diagnosed
Your eye doctor will:
- Take a detailed history of onset, number, and associated flashes or vision loss.
- Perform a dilated fundus examination to inspect the vitreous and retina for tears, holes, or bleeding.
- Use optical coherence tomography (OCT) to capture high-resolution cross-section images of the retina if macular pathology is suspected.
- Employ B-scan ultrasound when view is obscured by dense floaters or hemorrhage.
Most floaters are benign, but these tests rule out emergent problems such as retinal detachment, vitreous hemorrhage, or uveitis.
Why it happens: causes and risk factors
As we age, two parallel changes occur:
- Vitreous liquefaction and shrinkage – the once-gelatinous vitreous becomes more watery and pockets of liquid form.
- Weakening of vitreoretinal adhesion – the connective tissue that anchors the vitreous to the retina loosens, allowing clumps of collagen to float free.
Additional risk factors include:
- Nearsightedness over −6.00 D
- Posterior vitreous detachment in the fellow eye
- Previous cataract or YAG laser surgery
- Ocular trauma or inflammation
- Diabetic retinopathy or other vascular retinopathies
- Rapid shifts in blood sugar or blood pressure
Although floaters are common after age 50, younger adults with high myopia or athletes suffering blunt eye trauma may also notice them.
Conventional treatment options
Most floaters require only reassurance and periodic observation. When they severely impair vision or quality of life:
- YAG laser vitreolysis – a laser vaporizes clumps suspended in the mid-vitreous. Best for discrete solitary floaters and clear ocular media.
- Pars plana vitrectomy – surgical removal of the vitreous gel and replacement with balanced salt solution. Highly effective but carries small risks of cataract, retinal detachment, and infection.
- Monitor for complications – sudden increase in floaters, flashes, or side-vision shadow mandates same-day examination because early repair of a retinal tear dramatically lowers detachment risk.
Eye Health Institute’s integrative approach
At the Eye Health Institute we address floaters by supporting the overall health of the vitreous and retina instead of simply chasing each new speck.
Key modalities
- Micro Acupuncture 48 improves microcirculation to nourish the retina and speed clearance of vitreous debris.
- Microcurrent stimulation (ACS-3000) delivers gentle electrical signals that may enhance ocular metabolism and collagen remodeling.
- Targeted herbal and nutritional formulas provide antioxidants (vitamin C, lutein, zeaxanthin) and collagen cofactors (vitamin C, proline) to stabilize connective tissue.
- Hydrogen-rich water therapy combats oxidative stress in the vitreous.
- Lifestyle counseling emphasizes hydration, anti-inflammatory diet, stress reduction, and limiting high-impact activities that jolt the vitreous.
- At-home maintenance programs blend remote coaching, tele-review of symptoms, and periodic office intensives for personalized care.
Our goal is not only to calm existing floaters but also to reduce the likelihood of sudden increases by keeping the vitreous environment healthy.
What patients report / clinical insights
Long-time clinic patients often describe floaters as “less noticeable” after a series of microcurrent and acupuncture sessions. Some learn to ignore remaining floaters more easily, while others see gradual fading over months. Education on warning signs and prompt communication with our doctors forms a cornerstone of every treatment plan.

When to seek urgent care
Seek emergency eye care immediately if you notice:
- A sudden burst of many new floaters or “pepper flakes”
- Bright flashes of light in side vision
- A dark curtain, veil, or shadow moving across any part of your vision
- Eye pain with floaters or loss of vision
These symptoms can indicate a retinal tear or detachment, vitreous hemorrhage, or other sight-threatening events. Call your ophthalmologist or visit an emergency eye clinic without delay. Learn more about related issues such as retinal detachment and vitreous detachment.
Get urgent eye care for sudden vision loss, a curtain or shadow, new flashes with many floaters, severe eye pain, or eye trauma. These can be emergencies.