Eye Condition
Uveitis
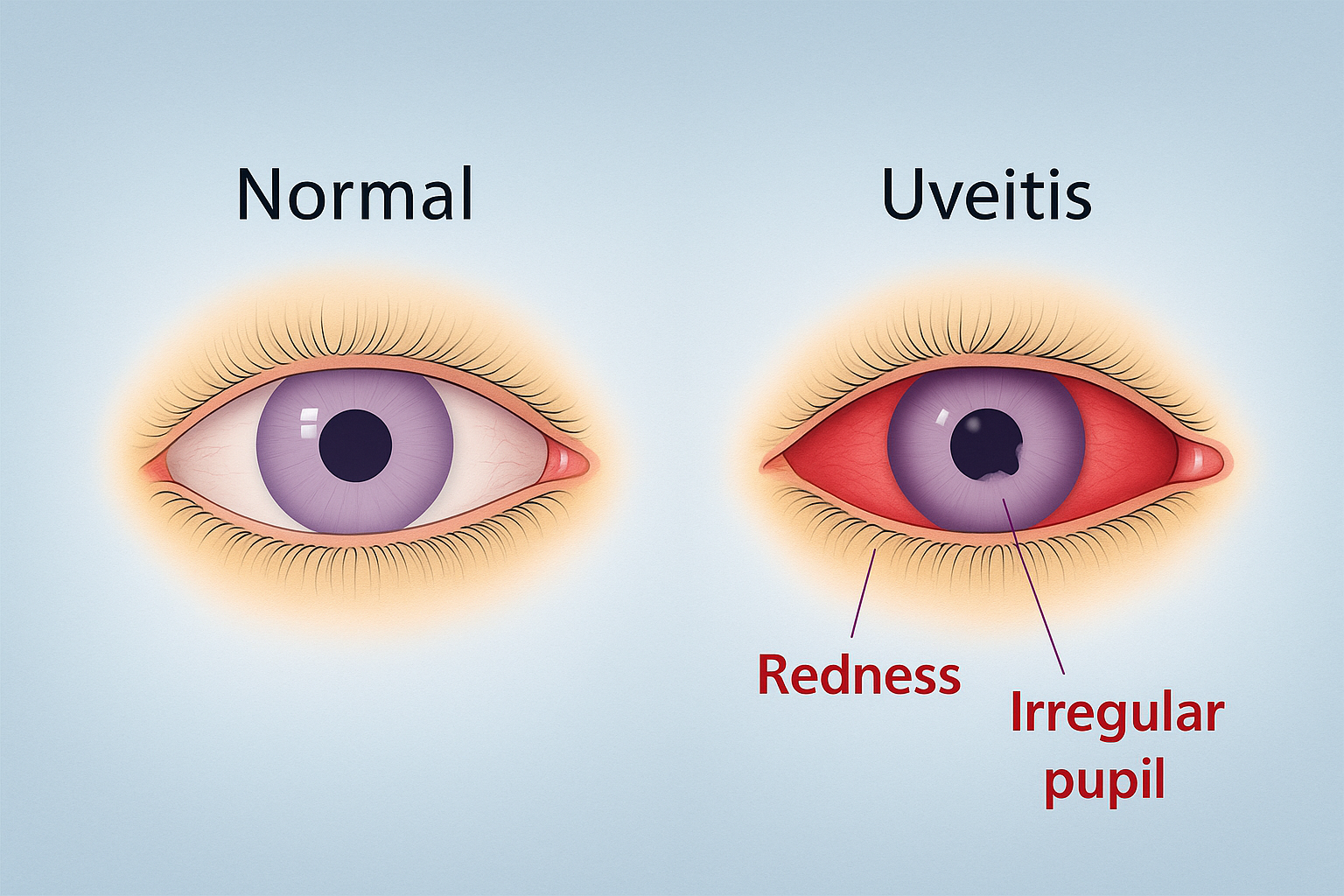
Uveitis is inflammation inside the eye’s middle layer that can cause redness, pain, and blurred vision, potentially leading to permanent damage without prompt care.
Explore our treatment options for Uveitis
What is Uveitis?
Uveitis is an inflammatory condition that affects the uveal tract (iris, ciliary body, choroid) and sometimes the adjacent retina or optic nerve. It may be anterior (iritis), intermediate, posterior, or panuveitis, and it can occur in one or both eyes. Flares may be sudden or gradual, mild or vision-threatening. At the Eye Health Institute (EHI) we see uveitis most often in the context of systemic or localized autoimmune activity, although infections, trauma, and certain medications can also trigger it.
Key symptoms and early warning signs
- Eye redness that does not clear with rest
- Deep aching or light-sensitive eye pain
- Blurred or hazy vision
- Floating spots or flashes of light
- New or worsening light sensitivity
- In children, a painless flare may be silent; routine eye exams are critical
How Uveitis is diagnosed
Your ophthalmologist will examine the front and back of the eye with a slit lamp and dilated fundus exam. Optical coherence tomography (OCT) can reveal subtle macular swelling, while fluorescein or indocyanine angiography maps hidden leakage. Blood tests, chest X-ray, or imaging may search for underlying infections, sarcoidosis, or systemic autoimmune disease. At EHI we also review gut health markers and vitamin D status because they influence immune balance.
Why it happens: causes and risk factors
More than one-third of uveitis cases are linked to autoimmune disorders such as ankylosing spondylitis, juvenile idiopathic arthritis, psoriasis, or inflammatory bowel disease. Viral and bacterial infections (herpes, toxoplasmosis, tuberculosis) may provoke secondary inflammation. Other contributors include:
- Recent eye surgery or trauma
- Smoking and high systemic oxidative stress
- Imbalanced gut microbiome (dysbiosis) that stirs systemic inflammation
Family history, certain HLA gene markers, and low vitamin D add to risk. Persistent inflammation can raise eye pressure and mimic glaucoma.
Conventional treatment options
Standard care begins with topical corticosteroid drops for anterior uveitis. More stubborn or posterior cases often require peri-ocular or oral steroids, immunosuppressive agents (methotrexate, mycophenolate, adalimumab), or biologics guided by a rheumatologist. Cycloplegic drops ease pain from ciliary spasm. These medicines can be lifesaving; however, long-term use may elevate cataract or glaucoma risk and does not address dietary or lifestyle triggers of autoimmunity.
Eye Health Institute’s integrative approach
Dr. Rosenfarb’s team works alongside your ophthalmologist to help the eye and immune system find a steadier state of remission. Key elements include:
Micro Acupuncture 48 & electro-microcurrent (ACS-3000)
Targeted needling plus gentle microcurrent around ocular regions may improve local circulation and neuro-immune signaling.
Herbal and nutritional therapy
Customized formulas rich in curcumin, omega-3s, and mitochondrial cofactors support antioxidant defenses while dampening inflammatory cytokines. Molecular hydrogen (H2) tablets or inhalation goggles are offered to counter oxidative stress revealed in recent EHI research.
Gut-eye axis care
Because “a healthy gut is a healthy brain and eye,” we screen for dysbiosis, leaky-gut patterns, and food sensitivities. Probiotics, short-term elimination diets, or digestive botanicals can rebalance the microbiome that shapes systemic immunity.
Stress modulation & lifestyle coaching
Breathwork, moderate exercise, and sleep hygiene quiet overactive sympathetic pathways shown to worsen flares.
Intensive one-week in-clinic programs combine these modalities for rapid stabilization, followed by at-home kits so patients maintain progress between check-ins.
Remission is the key word here; we help optimize your health so your immune system is not hyperactive and attacking the structures of your eyes.
What patients report / clinical insights
Many patients arrive feeling isolated after years of cycling steroids. Community makes a difference. By connecting inside EHI groups they discover others on the same path, share anti-inflammatory recipes, and celebrate small wins such as longer intervals between flares or sharper contrast sensitivity. Clinical records show that patients who address gut health, manage stress, and follow home microcurrent protocols tend to taper steroids more comfortably under their doctor’s supervision.

You are not alone; join our community and connect with positive people who are dealing with the same challenges.
When to seek urgent care
Get urgent eye care for sudden vision loss, a curtain or shadow across vision, many new floaters with flashes, severe eye pain, intense redness after injury, or any rapid change in light sensitivity. These can be emergencies.