Eye Condition
Central Serous Retinopathy
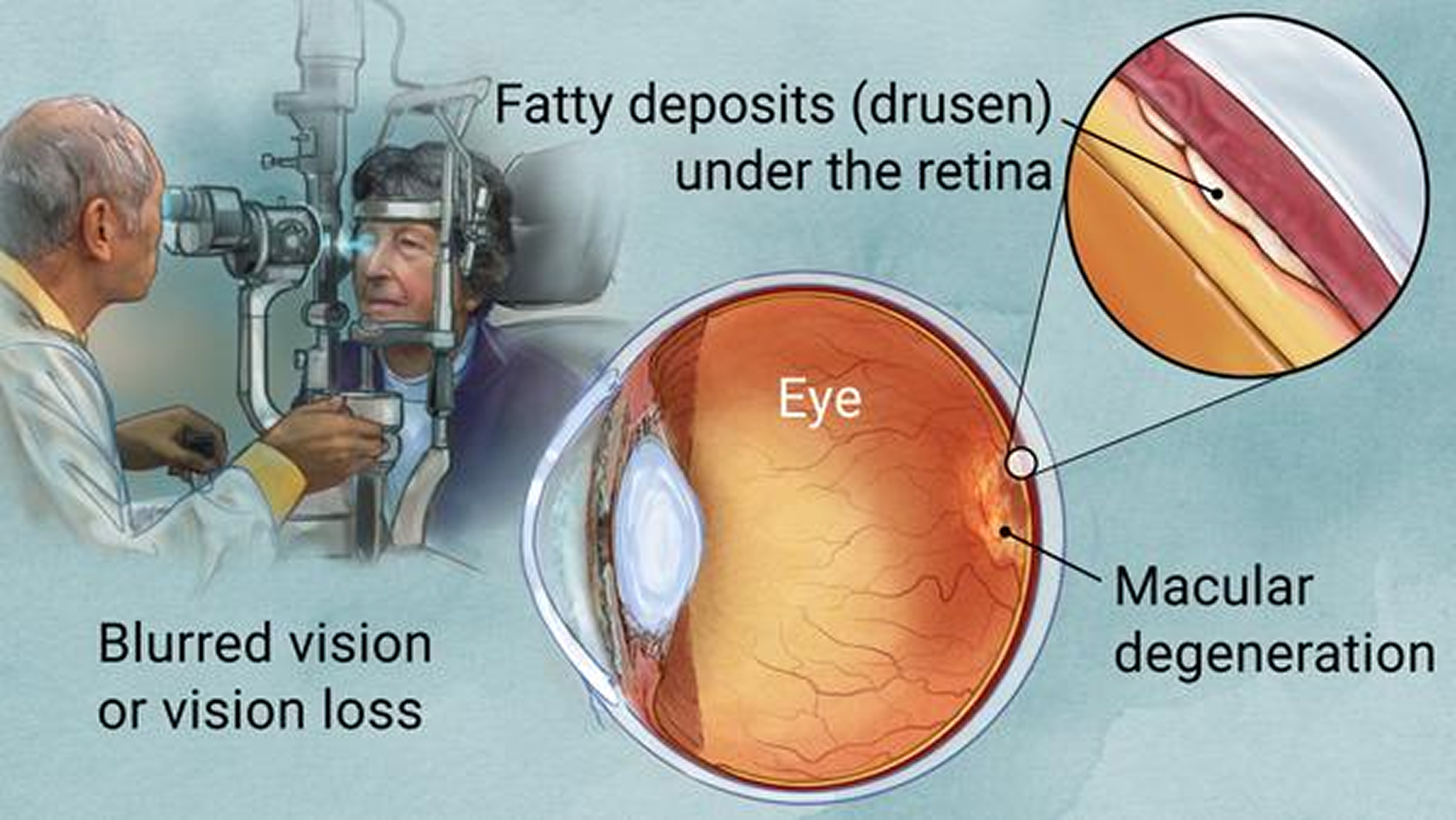
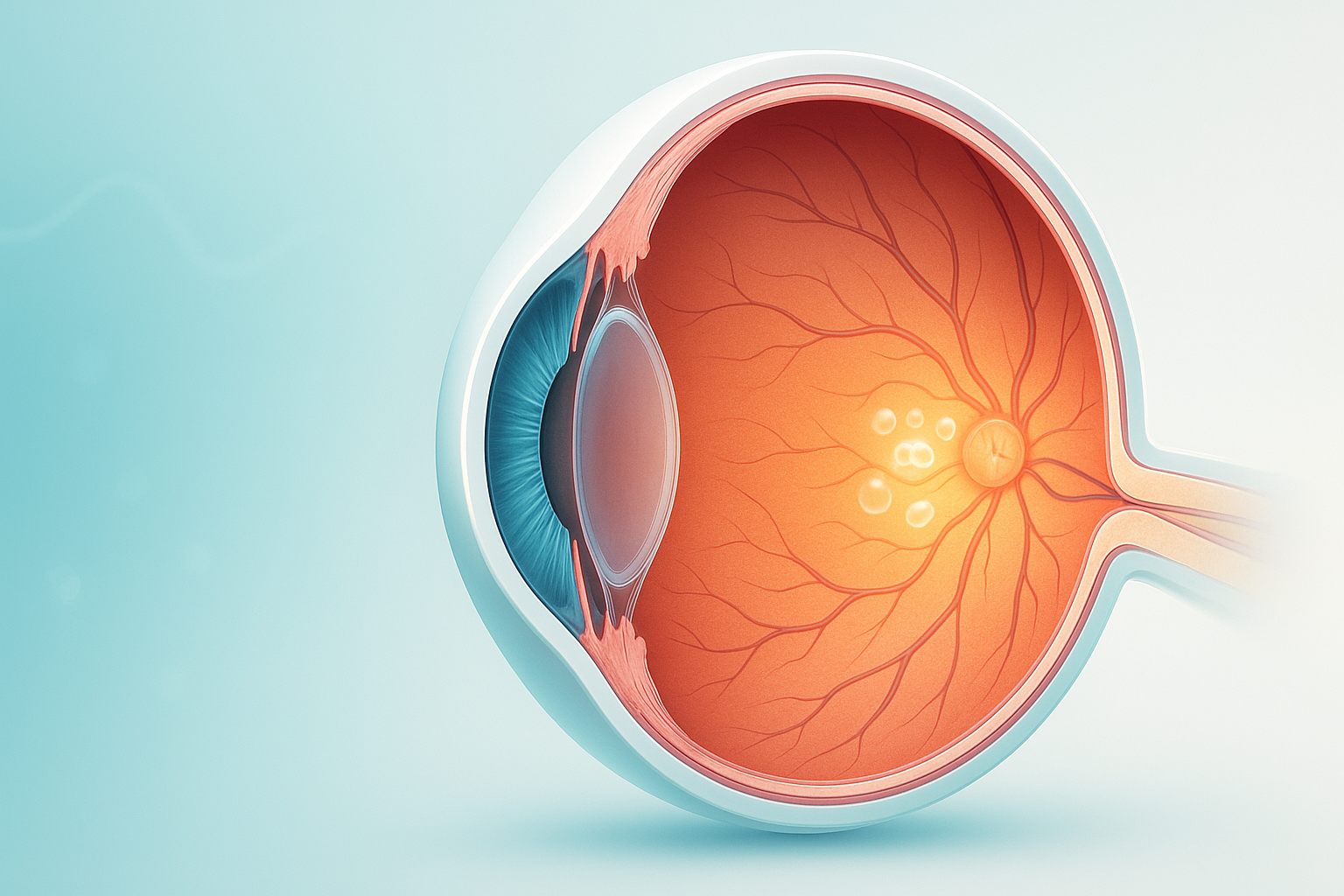
Central serous retinopathy is a condition that causes fluid to leak from the choroid layer into the macula, causing blurring or distortion of central vision.
Explore our treatment options for Central Serous Retinopathy
Overview
Central Serous Chorioretinopathy (sometimes called Central Serous Retinopathy) occurs when fluid from the choroid seeps through tiny defects in the retinal pigment epithelium (RPE) and accumulates under the neurosensory retina. The resulting blister‑like pocket lifts the central macula, causing sudden blurred, distorted, or dim central vision. Most patients are otherwise healthy men aged 20-50, but the condition can affect women and older adults, especially in chronic or recurrent forms.
Causes & Risk Factors
Systemic factors
- High psychological stress or “type-A” personality traits
- Elevated glucocorticoids (oral, inhaled, topical, anabolic)
- Cushing syndrome
- Pregnancy
- Hypertension
- Obstructive sleep apnea
Ocular factors
- High sympathetic tone
- “Pachychoroid” anatomy (thickened choroid with dilated vessels)
- Previous episode of CSC
Demographic factors
- Male sex (about 70-80% of cases)
- Age 20-50 years
- Higher prevalence in Asian and Hispanic populations
Genetic or experimental factors
- Variants in mineralocorticoid and complement pathways (under study)
Pathophysiology
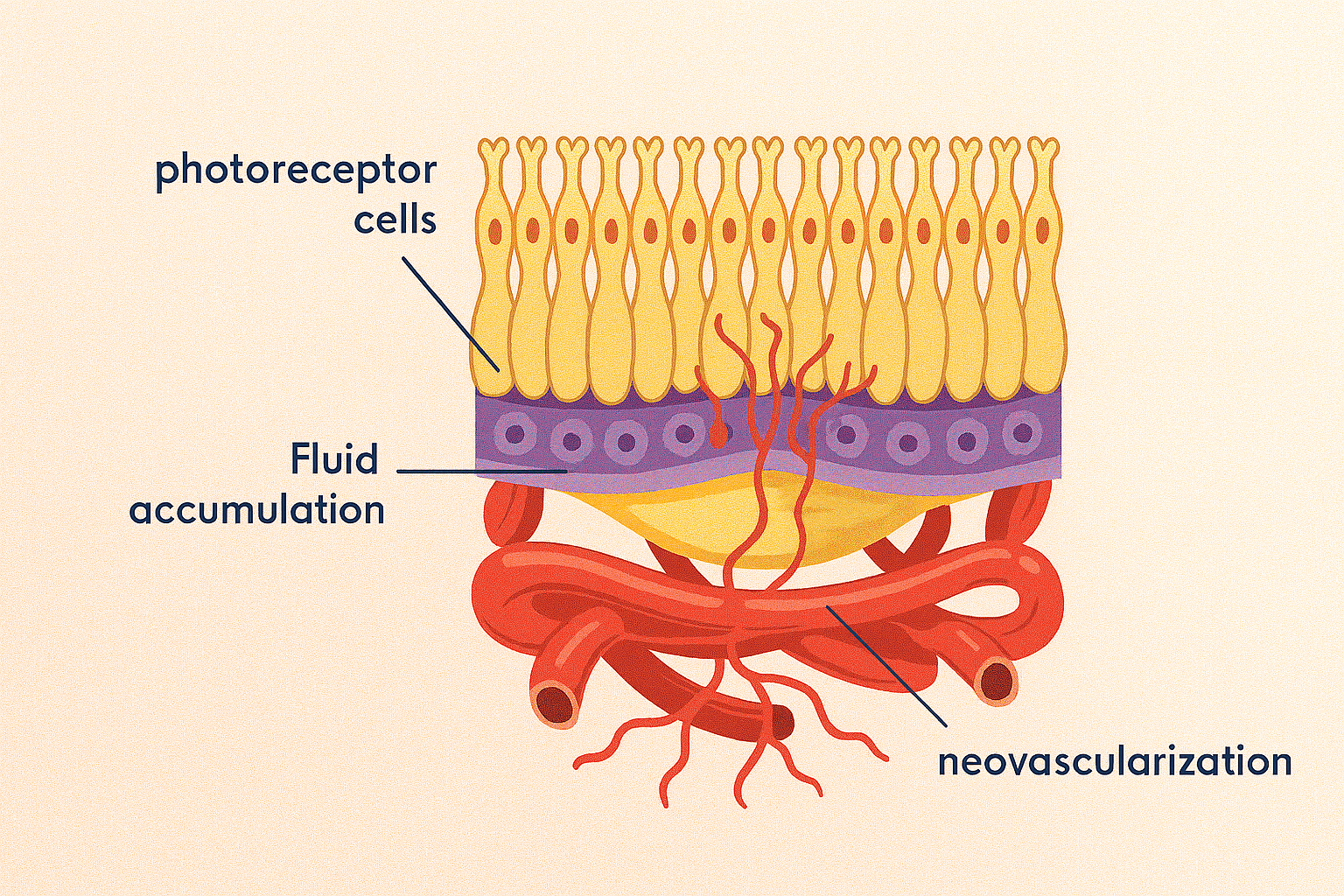
Modern imaging points to widespread choroidal hyper-permeability and congestion. These vascular changes overload the RPE’s pumping capacity, creating microscopic breaks through which serous fluid seeps. Once the RPE barrier fails, fluid pools under the macula until intrinsic healing or external intervention restores the barrier.
Signs & Symptoms
- Sudden blurred or “foggy” central vision (usually in one eye)
- Straight lines look bent or smaller than normal (micropsia)
- Colors appear faded or washed-out
- Faint gray spot or blind spot in the center of vision
- Typically painless, and symptoms may fluctuate over hours or days
Diagnostic Work-up
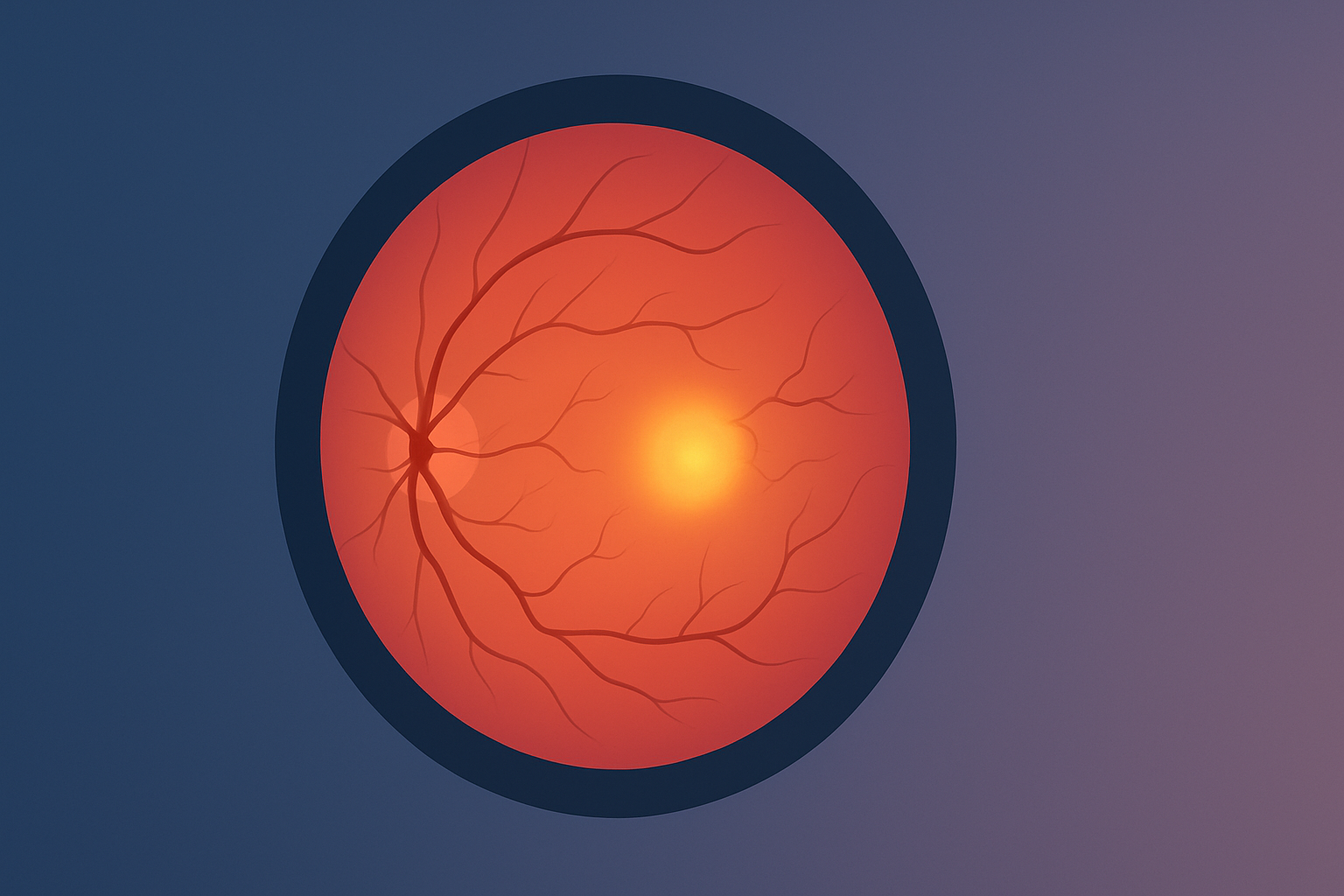
Optical Coherence Tomography (OCT)
Reveals a dome-shaped neurosensory detachment with sub-retinal fluid and often a thickened choroid.
Fluorescein Angiography (FA)
Shows classic “smoke-stack” or “ink-blot” leakage patterns that confirm focal RPE leaks.
Indocyanine Green Angiography (ICGA)
Highlights larger areas of choroidal hyper-permeability and vascular congestion.
OCT-Angiography and Fundus Autofluorescence
Provide non-invasive insights into choroidal flow and stress on the RPE.
Natural History
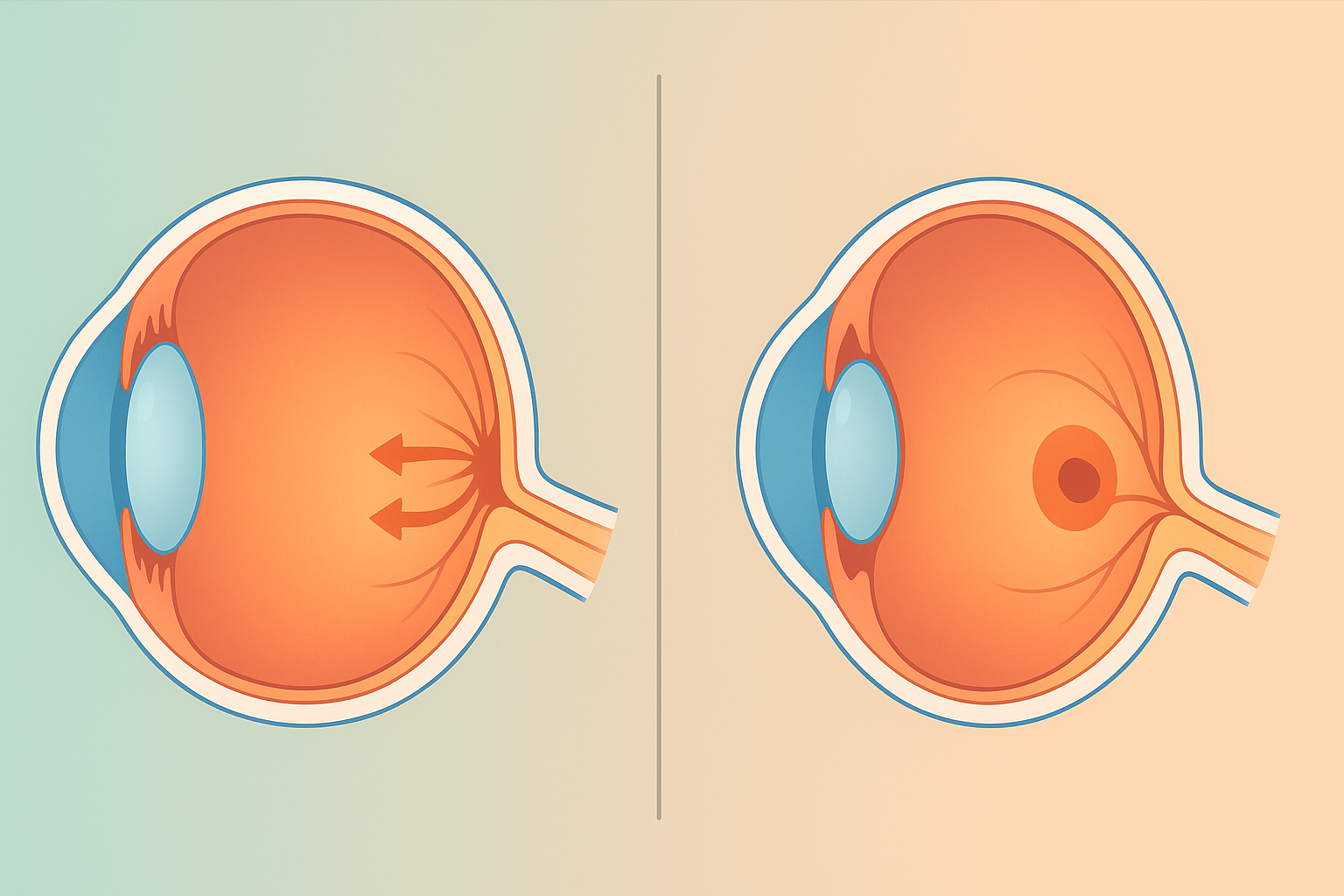
Acute CSC
- Fluid typically resolves within 3-4 months.
- About 80% of patients recover near-baseline sharpness, though mild contrast-sensitivity loss can persist.
Chronic or Recurrent CSC
- Defined by fluid persisting longer than 4-6 months or by repeated episodes.
- Ongoing detachment risks RPE atrophy and permanent visual loss.
Prognosis
Most acute cases return to 20/25 vision or better once the fluid clears. In chronic disease, visual acuity often stabilizes around 20/40-20/60, and long-standing fluid can permanently reduce contrast sensitivity or color perception. The single best predictor of outcome is the length of time the macula remains detached—the shorter the duration, the better the long-term vision.
Key Takeaways
- CSCR is a self-limited macular detachment driven by choroidal hyper-permeability and RPE dysfunction.
- Young, healthy patients often recover spontaneously, but chronic or recurrent disease carries a risk of lasting visual loss.
- Regular OCT monitoring—typically every 4-6 weeks—helps distinguish resolving acute episodes from cases that may require intervention.
- Reducing systemic risk factors, especially steroid exposure and stress, lowers the chance of recurrence and safeguards long-term vision.