Eye Condition
Retinal Occlusion (Eye Stroke)
Retinal occlusion, also known as an eye stroke, happens when a blocked artery or vein suddenly stops blood flow to the retina, causing rapid vision loss.

Explore our treatment options for Retinal Occlusion (Eye Stroke)
What Is Retinal Occlusion (Eye Stroke)?
Retinal occlusion, often called an eye stroke, happens when a blood vessel in the retina becomes blocked. The interruption stops normal circulation, starves the tissue of oxygen, and triggers bleeding or swelling that can rob you of vision in minutes or hours.
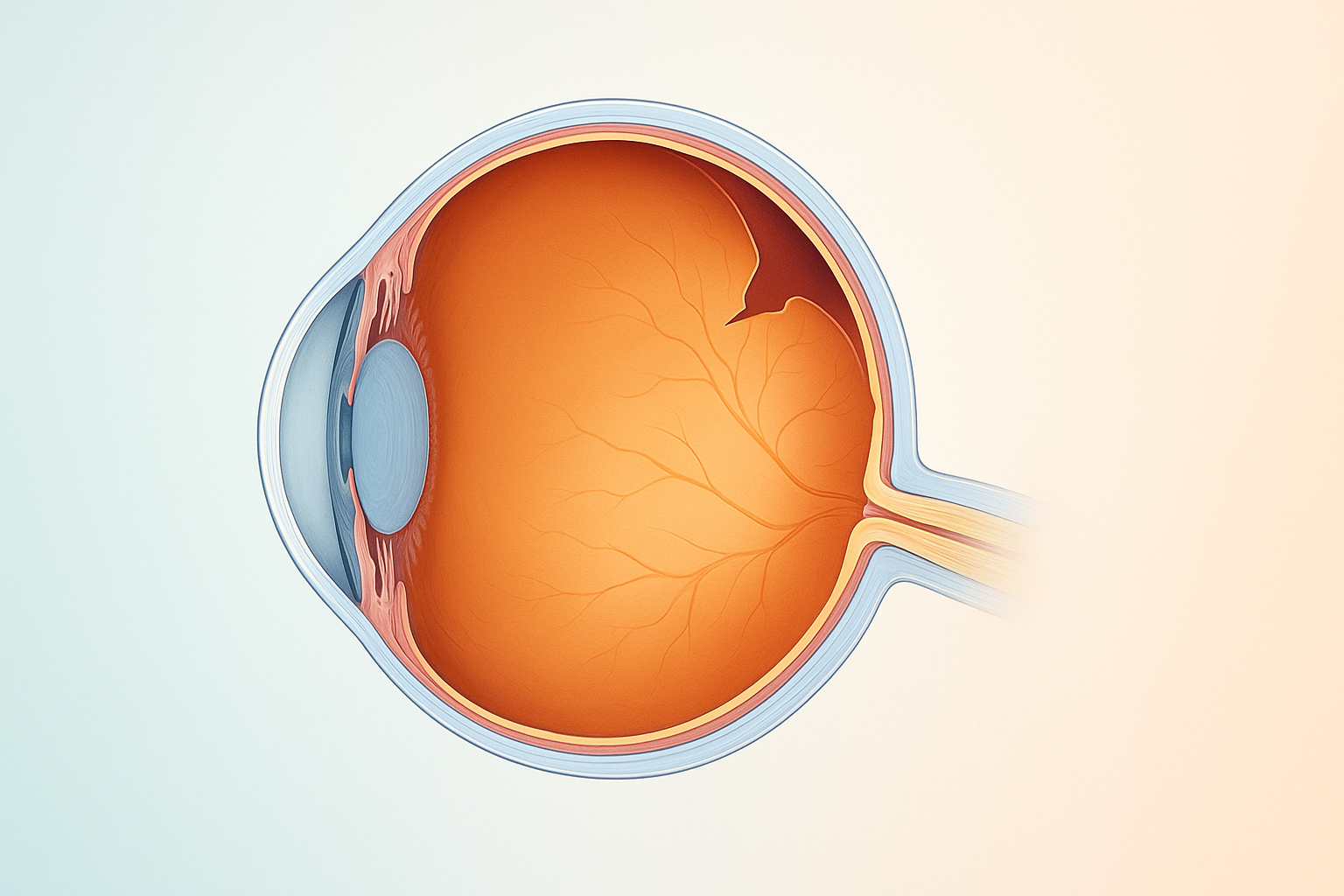
How Retinal Blood Flow Normally Works
The retina relies on two tiny plumbing systems:
- Retinal arteries deliver oxygen-rich blood from the heart.
- Retinal veins drain oxygen-depleted blood back toward the heart.
When either system stalls, waste builds up and light-sensitive cells begin to die. Vein blockages are far more common than arterial blockages, but both demand urgent care.
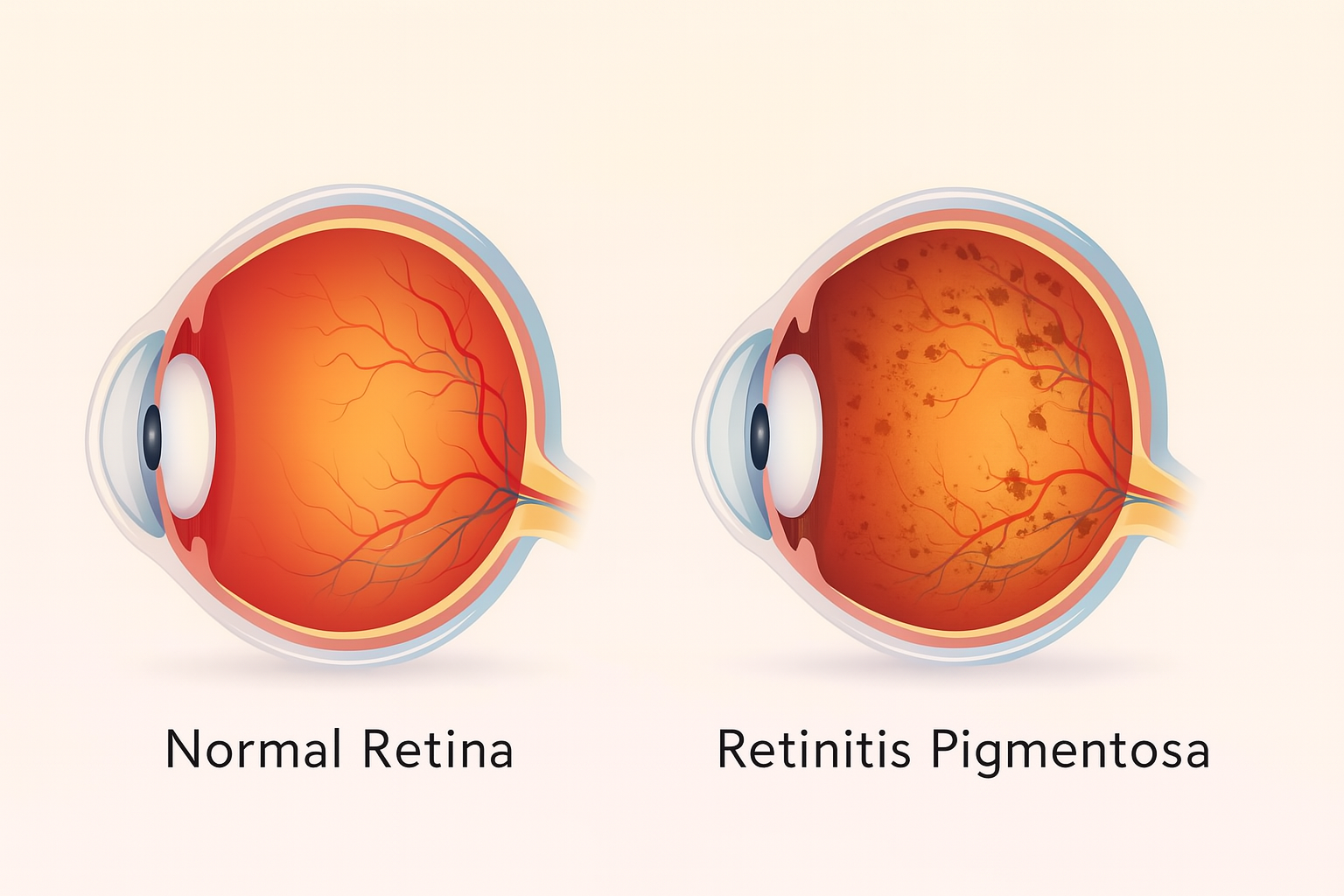
What Happens When a Vein Is Blocked?
A neighboring hardened artery may press on a vein, creating turbulence, clot formation, and finally a full obstruction. Blood backs up, pressure rises, and small vessels rupture. The result is scattered hemorrhages and fluid leakage that blur or darken vision without pain.
Types of Retinal Vein Occlusion
Blockages are grouped by location and the amount of oxygen deprivation they cause. Understanding the difference guides prognosis and treatment.
Non‑Ischemic (Venous Stasis Retinopathy)
- Accounts for 75 to 80 percent of cases.
- Circulation slows but alternative channels form, limiting tissue damage.
- Macular edema (swelling in the central retina) may develop, yet neovascularization — growth of fragile new vessels — is uncommon.
- Vision often remains stable or improves with proper management.
Ischemic (Hemorrhagic Retinopathy)
- A complete or near‑complete shutdown of blood flow.
- Severe oxygen shortage leads to large hemorrhages, extensive macular edema, and widespread capillary dropout.
- Two‑thirds of patients risk profound, permanent vision loss.
- Neovascularization can sprout on the retina, iris, or optic nerve, raising the danger of glaucoma and recurrent bleeding.
Signs and Symptoms You Should Never Ignore
- Sudden, painless loss of vision in one eye
- Blurry or dimmed central vision
- A dark or empty spot in the visual field
- Distorted or wavy lines (metamorphopsia)
- Floaters that resemble tiny red or black specks
Because retinal tissue lacks pain receptors, a dramatic change in sight may be the only clue that an occlusion is underway.
Who Is Most at Risk?
- High blood pressure: Damages vessel walls and accelerates clot formation
- High cholesterol: Promotes artery hardening that can compress veins
- Diabetes: Thickens vessel walls and alters blood viscosity
- Smoking: Constricts blood flow and raises clot risk
- Glaucoma: Elevates internal eye pressure that can impede venous return
- Blood clotting disorders: Increase the chance of occlusive events
- Age over 50: Vessels naturally stiffen over time
Diagnostic Tests Your Eye Doctor May Use
- Dilated fundus examination - allows direct viewing of retinal hemorrhages and edema.
- Optical coherence tomography (OCT) - cross-sectional scans reveal fluid, swelling, or macular thickening.
- Fluorescein angiography - highlights blocked or leaking vessels and maps ischemic zones.
- Ocular ultrasound - evaluates deeper hemorrhages if the view is clouded.
- Blood work and blood pressure check - identifies systemic contributors such as hypertension, diabetes, or clotting abnormalities.
Evidence‑Based Treatment Options
Anti-VEGF injections: First-line therapy that shrinks abnormal vessels and reduces macular edema. Most patients need monthly injections for several months, then taper to maintenance visits.
Steroid implants or injections: Control stubborn swelling when anti-VEGF response is limited. They carry a higher risk of cataract progression and elevated eye pressure, so monitoring is essential.
Laser photocoagulation: Seals leaky capillaries, shrinks ischemic zones, and lowers the risk of neovascular glaucoma. Focal laser targets the macula, while pan-retinal laser treats the peripheral retina.
Systemic management: Tight control of blood pressure, blood sugar, and cholesterol limits further vascular damage. Your ophthalmologist may coordinate care with a primary doctor or cardiologist.
Surgery for complications: Vitrectomy removes persistent hemorrhage or clears a dense vitreous clot that obscures vision.
What to Expect During Recovery
Vision recovery depends on the extent of ischemia, timing of treatment, and individual health. Non-ischemic occlusions can stabilize or improve within weeks, while ischemic events may leave lasting blind spots. Consistent follow-up is vital, as re-occlusion or neovascular complications can arise months later.
Lifestyle Habits That Protect Retinal Health
- Adopt a heart-smart diet rich in vegetables, fruits, lean protein, and omega-3 fats.
- Exercise at least 150 minutes per week to improve vascular function and blood-sugar control.
- Keep blood pressure below 120/80 mmHg or your physician's recommended target.
- Quit smoking and limit alcohol to moderate levels.
- Monitor cholesterol and A1C through regular checkups, adjusting medication when needed.
- Wear protective eyewear during high-impact sports or hazardous work to avoid simultaneous trauma.
When to Seek Emergency Care
A suspected eye stroke is an urgent medical situation. If you notice a sudden drop in vision, flashes, or a curtain-like shadow, call your ophthalmologist or head to the nearest emergency department immediately. Early intervention improves the odds of preserving sight.
Key Takeaway
Retinal occlusion (sometimes called an eye stroke) blocks essential blood flow and can steal vision without warning. Know the risk factors, recognize the symptoms, and seek immediate specialist care. Prompt diagnosis, targeted eye injections or laser treatment, and disciplined systemic health management give you the best chance to protect and possibly restore your sight.
Learn More
Explore our comprehensive guides on eye stroke-related topics:
- AION (Anterior Ischemic Optic Neuropathy)
- BRAO (Branch Retinal Artery Occlusion)
- BRVO (Branch Retinal Vein Occlusion)
- Eye Stroke Causes
- Eye Stroke and COVID-19
- CRAO (Central Retinal Artery Occlusion)
- CRVO (Central Retinal Vein Occlusion)
- Eye Stroke and Diabetes
- Early Intervention for Eye Stroke
- Eye Stroke Exercises
- NAION (Non-Arteritic Anterior Ischemic Optic Neuropathy)
- Natural Treatments for Eye Stroke
- Eye Stroke Prevention
- Treatment Modalities for Eye Stroke
- Eye Stroke vs Brain Stroke