Eye Condition
Stargardt Syndrome
Stargardt syndrome is an inherited juvenile macular degeneration caused by gene mutations, leading to gradual central vision loss.

Explore our treatment options for Stargardt Syndrome
What is Stargardt syndrome?
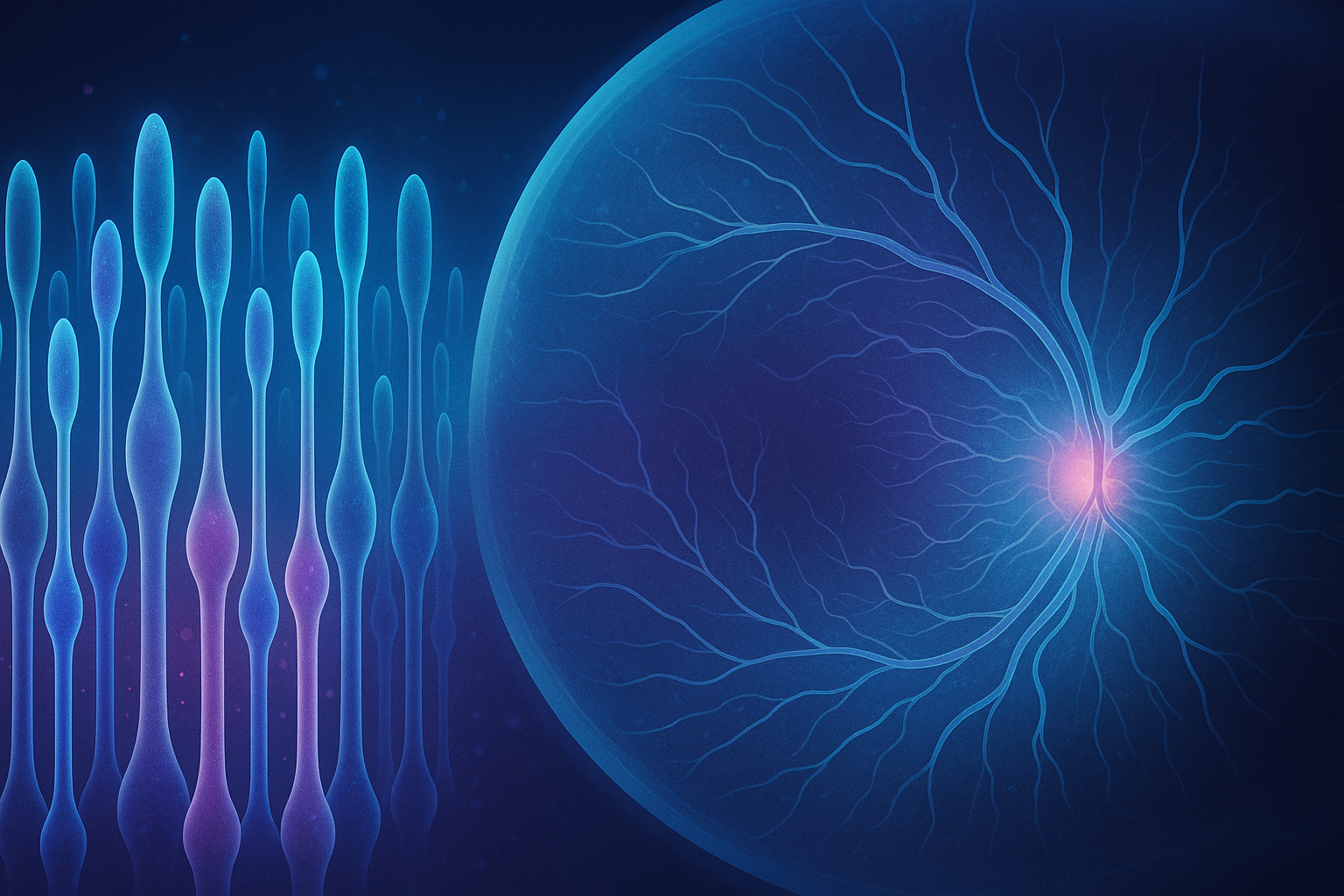
Stargardt syndrome (also called fundus flavimaculatus or Stargardt macular dystrophy) is the most common inherited form of juvenile macular degeneration. Caused by mutations in the ABCA4 gene, it prevents photoreceptor cells from properly clearing vitamin A by-products. Over time these by-products build up as yellowish lipofuscin deposits that damage the macula, the part of the retina responsible for sharp, color, and reading vision. Most people notice symptoms during late childhood to young adulthood, but progression is highly variable and can level off for years before accelerating.

Key symptoms and early warning signs
- Slow decline in sharpness of central vision
- Difficulty seeing in dim light or at dusk
- Trouble reading small print even when distance vision seems normal
- Washed-out or dull colors
- Small gray or blurry spots near the center of vision
- Sensitivity to bright light or glare
- Visual distortions such as straight lines appearing wavy
- In advanced stages, phantom images or simple visual hallucinations as the brain “fills in” missing detail
Early signs can mimic other conditions such as Macular Degeneration, so an eye exam with imaging is essential if any of these changes appear.
How Stargardt syndrome is diagnosed
Your EHI doctor will begin with a dilated retinal examination and high-resolution optical coherence tomography (OCT) to look for loss of photoreceptor layers. Fundus autofluorescence highlights lipofuscin flecks, while fluorescein angiography checks for atrophic patches. An electroretinogram (ERG) may be ordered to measure overall retinal function. Genetic testing confirms ABCA4 variants and helps differentiate Stargardt syndrome from cone-rod dystrophy or retinitis pigmentosa. Because childhood-onset vision problems can have many causes, a precise diagnosis guides both lifestyle choices and enrollment in research trials.
Why it happens: causes and risk factors
Stargardt syndrome follows an autosomal recessive inheritance pattern; both parents carry a silent copy of the ABCA4 mutation, giving each child a one-in-four chance of being affected. Researchers believe the faulty ABCA4 protein fails to shuttle vitamin A derivatives out of photoreceptors, leading to toxic buildup. High-dose vitamin A supplements may accelerate this buildup, so children with the disease should avoid megadose multivitamins unless advised by their physician. Although the condition is genetic, environmental stressors such as intense ultraviolet light, smoking, and poor nutrition may influence how quickly vision declines.
Conventional treatment options
There is currently no FDA-approved cure. Standard care focuses on slowing retinal stress and making the most of remaining sight:
- Low-vision rehabilitation, magnifiers, and digital devices
- Sunglasses with ultraviolet and blue-blocking filters
- Orientation and mobility training for school or work
- Monitoring for emerging therapies such as gene replacement, stem cell transplantation, and complement inhibitors now in clinical trials
- Genetic counseling for family planning
High-dose vitamin A palmitate, sometimes used in other retinal diseases, should not be taken. Clinical trials are exploring safer vitamin A analogs that do not form toxic by-products.
Eye Health Institute’s integrative approach
While continuing collaboration with your retinal specialist, EHI offers supportive therapies aimed at nourishing retinal cells, reducing oxidative stress, and promoting healthy blood flow:
- Micro Acupuncture 48: Targeted micro-needling protocols developed for macular degeneration aim to stimulate ocular circulation and nerve signaling.
- Electro-acupuncture and microcurrent stimulation: Gentle currents may enhance mitochondrial energy production in surviving photoreceptors.
- Nutritional counseling: Emphasis on dark leafy greens rich in lutein and zeaxanthin, omega-3 fatty acids, controlled vitamin A intake, and antioxidants such as alpha-lipoic acid.
- Herbal and nutraceutical support: Formulas featuring ginkgo biloba, bilberry, N-acetylcysteine, and coQ10 are selected case-by-case to address oxidative stress.
- Hydrogen therapy and light-blocking practices: Sessions with hydrogen-rich water or inhalation support antioxidant defenses, while blue-filter lenses limit phototoxicity.
- Stress-reduction and lifestyle coaching: Tailored breathwork, gentle movement, and sleep hygiene help modulate inflammatory pathways that can influence retinal health.
Our goal is not a cure promise, but rather to help stabilize functional vision, extend the usable visual field, and support overall quality of life alongside conventional care.
What patients report / clinical insights
Parents often tell us children feel less eye strain after several weeks of integrative therapy. Many patients notice reading comfort improves, even if the eye-chart line stays the same, because contrast sensitivity and adaptation to lighting are better. Adults appreciate strategies for screen ergonomics and tinted task glasses that reduce glare. Progress is evaluated every three to six months with OCT and functional testing so adjustments can be made promptly.

When to seek urgent care
Although Stargardt syndrome itself usually progresses gradually, retinal complications can still occur. Get urgent eye care right away if you experience any of the following:
- Sudden blackout or curtain over part of your vision
- A shower of new floaters with flashing lights
- Rapid worsening of central blurriness over hours or days
- Severe eye pain or redness after injury or contact lens wear
These events can signal a retinal tear, detachment, infection, or acute inflammation that needs same-day treatment to protect sight.