Eye Condition
Optic Neuritis
Optic neuritis is an immune-driven inflammation of the optic nerve that can cause sudden vision loss, eye pain, and color desaturation, yet many people recover well with timely, integrative care.
Explore our treatment options for Optic Neuritis
What is Optic Neuritis?
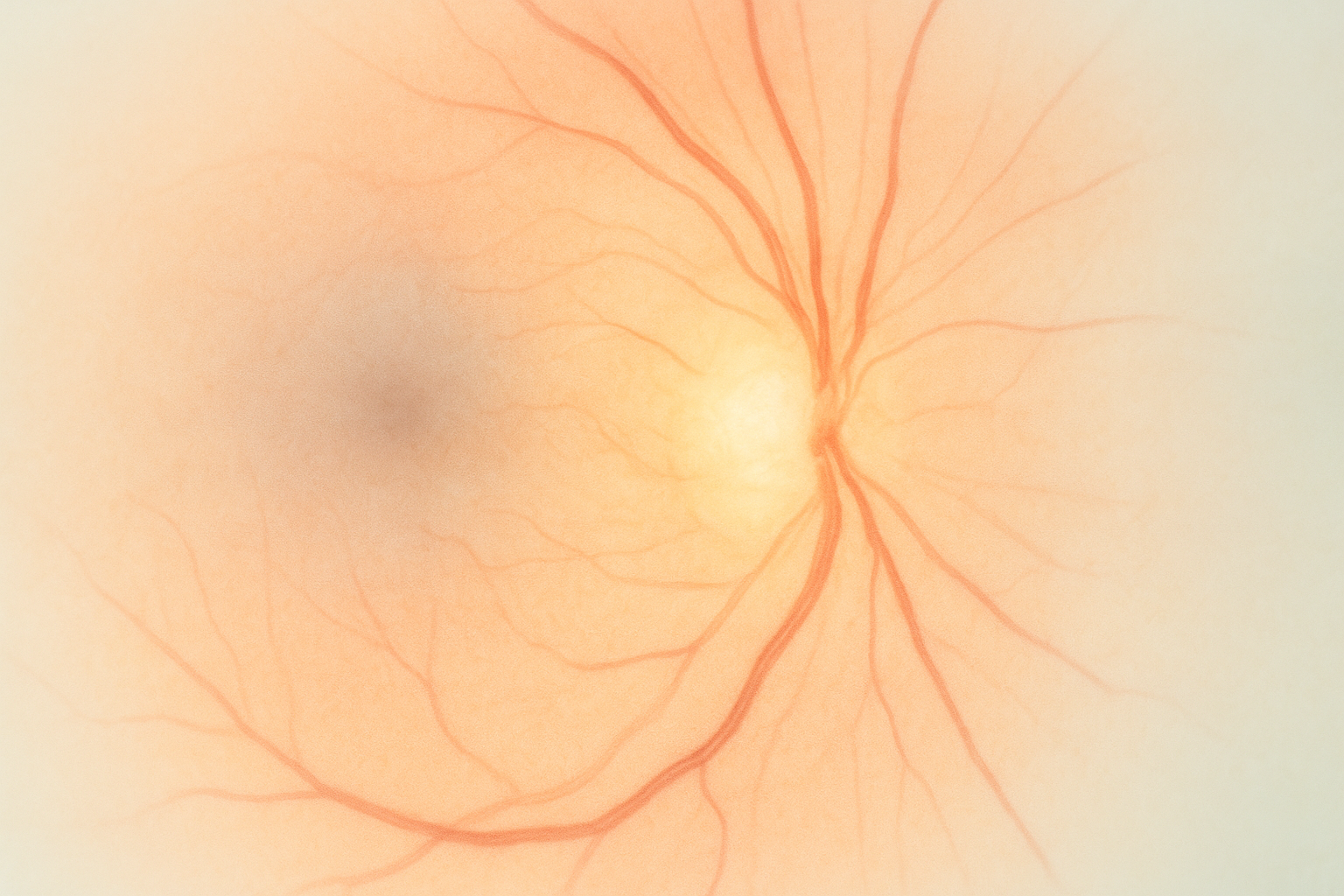
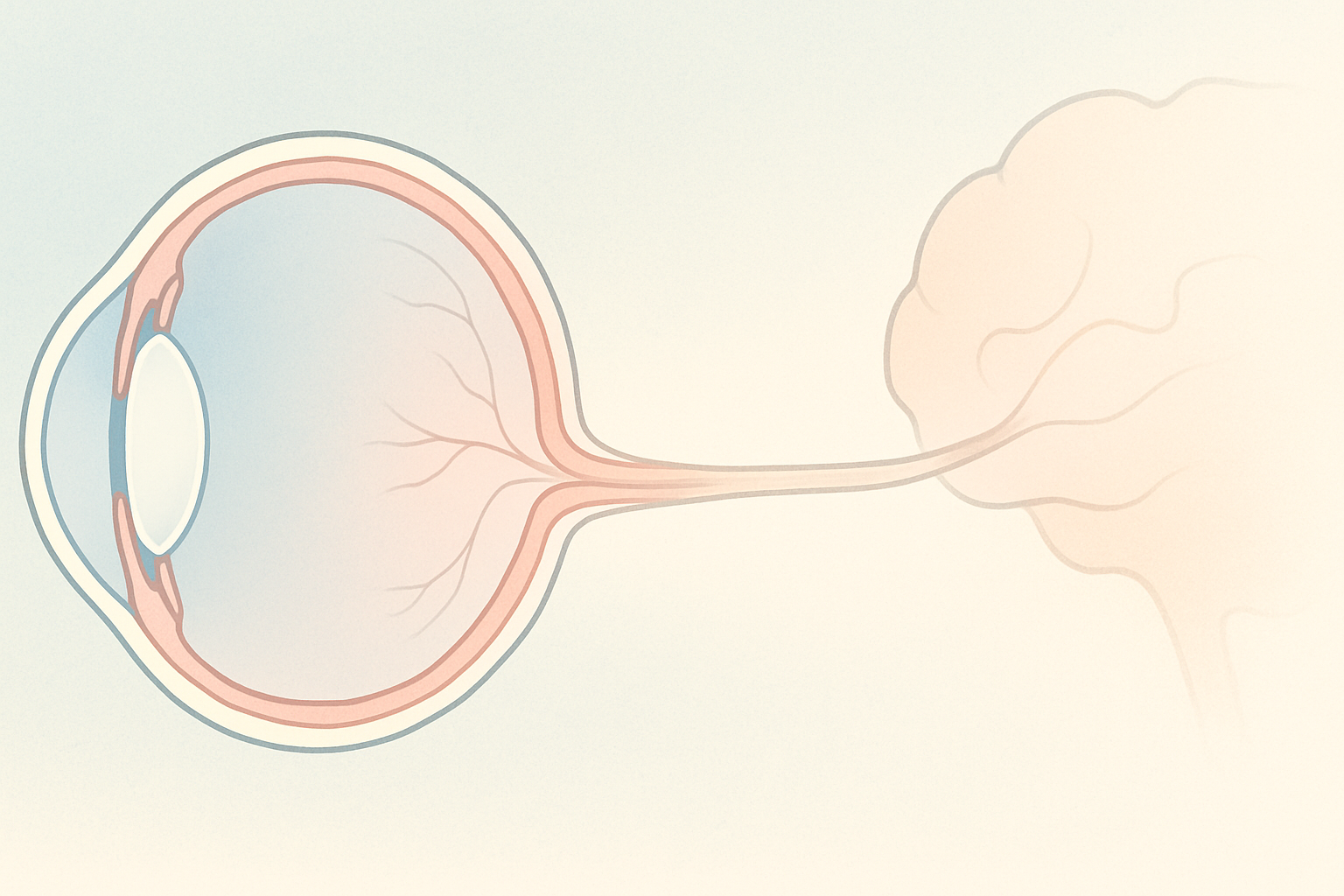
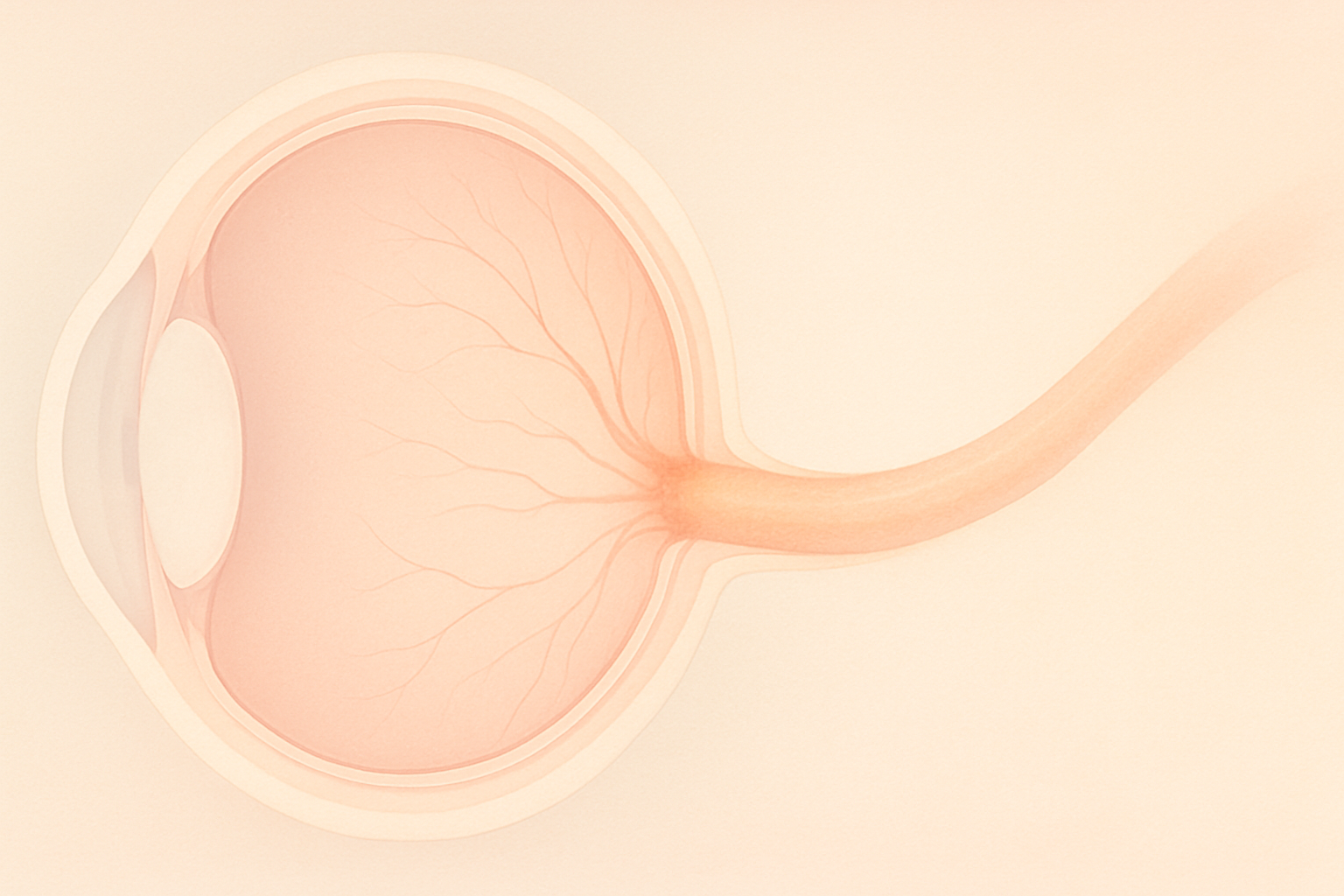
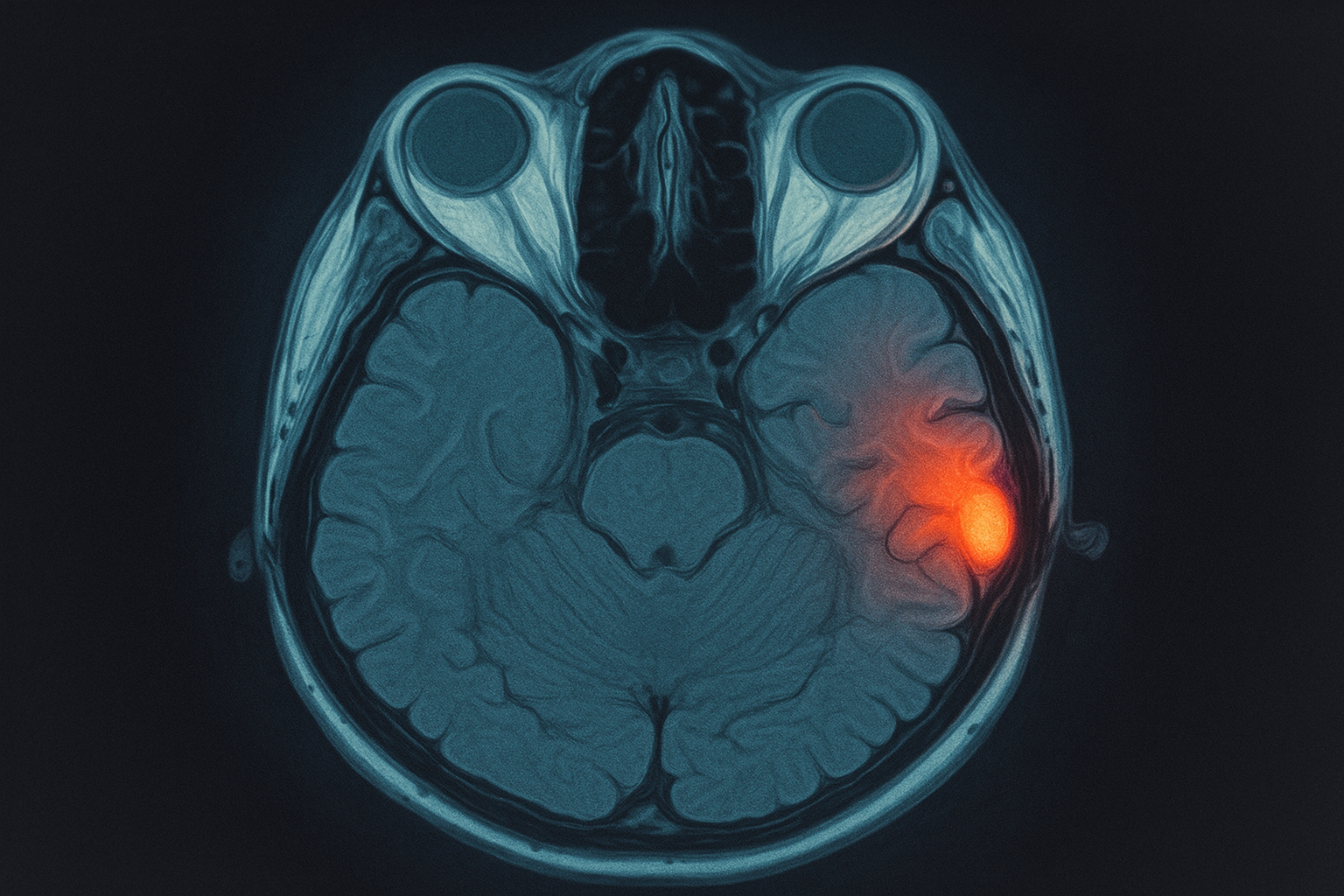
Optic neuritis is an acute or recurrent inflammation of the optic nerve, the million-fiber “data cable” that carries visual information from your retina to the visual cortex. When the nerve fibers or their insulating myelin sheath become inflamed, electrical signals slow or stop, and the brain receives incomplete images. Depending on which fibers are involved you may notice blurry central vision, dim colors, patchy peripheral vision, or reduced night vision. Although optic neuritis often improves over weeks to months, up to 20 percent of people develop lingering weakness in contrast or color perception, and repeated episodes can lead to permanent optic nerve atrophy.
Key symptoms and early warning signs
- Sudden or rapidly progressive blurry or dim vision in one eye
- Eye pain that worsens when you look side to side or up and down
- Colors, especially reds, appear washed out or gray
- Flashing lights or flickering when you move your gaze
- Diminished contrast and difficulty seeing at night
- Urgent sign: a relative afferent pupillary defect (your doctor sees one pupil constrict less to light) or loss of central vision within hours
How Optic Neuritis is diagnosed
Your eye doctor or neuro-ophthalmologist combines several tests to confirm inflammation and rule out other optic nerve problems:
- Comprehensive eye exam with visual acuity, color vision plates, and contrast sensitivity
- Swinging flashlight test for a pupillary defect
- Optical Coherence Tomography (OCT) to measure optic nerve fiber thickness
- Visual Evoked Potential (VEP) to check signal speed from eye to brain
- MRI of the orbits and brain with gadolinium to look for optic nerve swelling and plaques that suggest multiple sclerosis (MS)
- Blood work for infections, autoimmune antibodies, vitamin B 12 and folate, and markers of neuromyelitis optica spectrum disorder (NMOSD)
Why it happens: causes and risk factors
Most cases are autoimmune and demyelinating:
- Multiple sclerosis is detected in roughly 50 percent of first-time optic neuritis patients within 15 years.
- Neuromyelitis optica and MOG antibody disease produce more severe, bilateral attacks.
- Post-viral or post-vaccination immune reactions can trigger transient episodes.
- Infections (Lyme disease, syphilis, tuberculosis, viral encephalitis) occasionally inflame the nerve.
- Certain medications like ethambutol or amiodarone, toxic exposure to methanol, and severe vitamin B 12 deficiency can mimic the picture.
Women between 20 and 45 with a personal or family history of autoimmune disease carry the highest risk.
Conventional treatment options
- High-dose intravenous methylprednisolone (1 g daily for 3 days) followed by a short oral taper reduces inflammation and speeds visual recovery, though final acuity is often similar with or without steroids.
- Plasma exchange or IV immunoglobulin may be added for severe or steroid-resistant attacks, especially in NMOSD.
- Long-term disease-modifying therapy for MS lowers relapse rates.
- Treat underlying infection or nutritional deficiency when present.
- Neuro-protective vitamin D optimization, smoking cessation, and exercise are standard supportive measures.
Eye Health Institute’s integrative approach
Dr. Andy Rosenfarb and the EHI team combine mainstream neurology care with therapies that promote nerve healing and calm autoimmune activity:
| Modality | How it supports recovery |
|---|---|
| Micro Acupuncture 48 and peri-ocular acupuncture | Boosts local blood flow, modulates inflammatory cytokines, and may accelerate remyelination |
| Microcurrent stimulation (ACS-3000) | Provides gentle electrical cues that enhance mitochondrial energy production in damaged axons |
| Targeted herbal formulas (anti-inflammatory and neuro-protective botanicals, e.g., curcumin, astragalus) | Lower oxidative stress and stabilize myelin |
| Evidence-based nutraceuticals (omega-3, alpha-lipoic acid, methylated B-vitamins) | Supply critical cofactors for nerve repair |
| Hydrogen-rich water or tablets | Acts as a selective antioxidant targeting hydroxyl radicals that arise during acute inflammation |
| Infrared light therapy and gentle breathing exercises | Support circulation, reduce pain, and ease anxiety around sudden vision loss |
| Lifestyle coaching on gut-immune health, low-glycemic nutrition, and stress management | Addresses systemic triggers that can precipitate attacks |
In office, many patients complete a 5- to 10-day intensive program that layers two daily acupuncture sessions, microcurrent, and nutrition consults, followed by an at-home maintenance kit. Those unable to travel use telehealth to learn acupressure points, device settings, and supplement timing. EHI closely coordinates with your neurologist to ensure complementary rather than conflicting care.
What patients report / clinical insights
During follow-up surveys, a majority describe faster color return, brighter contrast, and less blind spot distortion compared with prior attacks that did not include integrative therapy. Some note improved energy, fewer headaches, and reduced fear about future relapses. Objective OCT scans often show better preservation of the retinal nerve fiber layer, aligning with peer-reviewed studies that link combined acupuncture and microcurrent to measurable neuro-protective effects. Consistency is key: the most durable gains occur in patients who keep up weekly home microcurrent, anti-inflammatory nutrition, and periodic booster acupuncture every three months.

When to seek urgent care
Get urgent eye care if you experience sudden vision loss, a dark curtain, new flashing lights with many floaters, severe eye pain, or any eye trauma. Quick evaluation and imaging are vital to protect your optic nerve and to direct you to the right neurologic or infectious work-up.
This information is for educational purposes and is not a substitute for one-on-one medical advice. Always consult your ophthalmologist or neurologist before making changes to your treatment plan.