Eye Condition
Macular Edema (Cystoid Macular Edema)
Macular edema, also called cystoid macular edema, is swelling in the retina’s center that blurs detail; our goal is early detection & integrative care to help protect sight.
Explore our treatment options for Macular Edema (Cystoid Macular Edema)
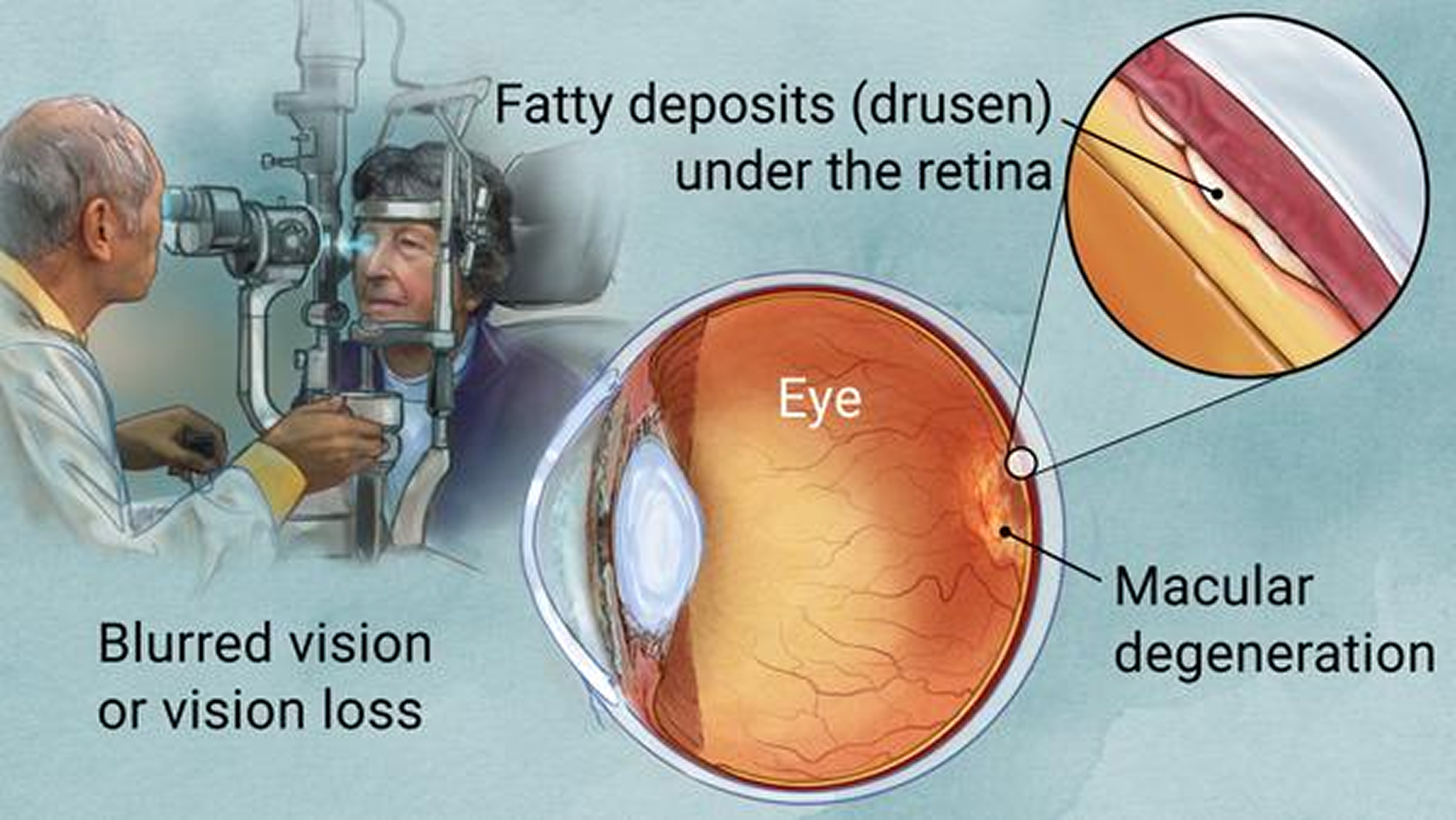
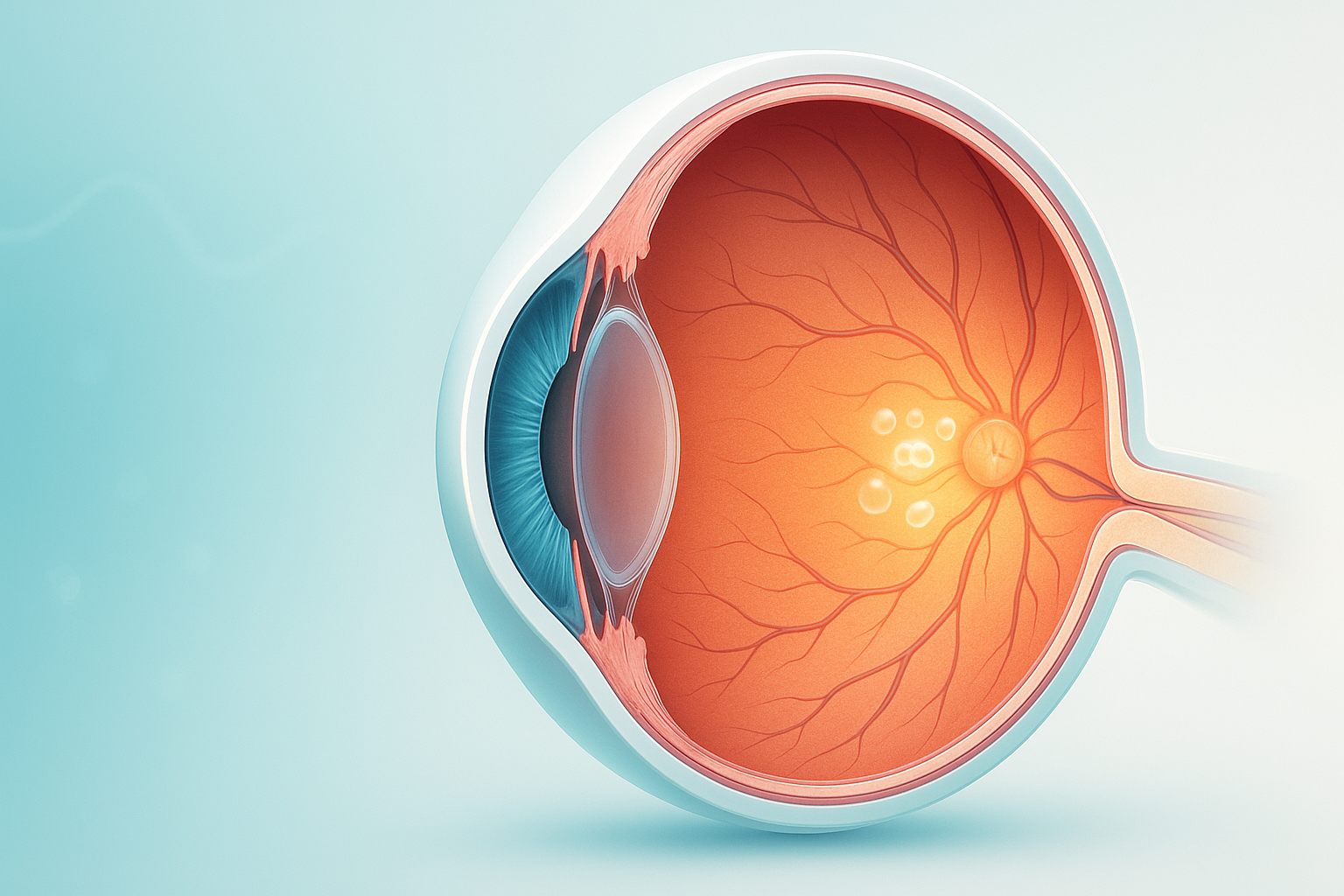
What is Macular Edema (Cystoid Macular Edema)?
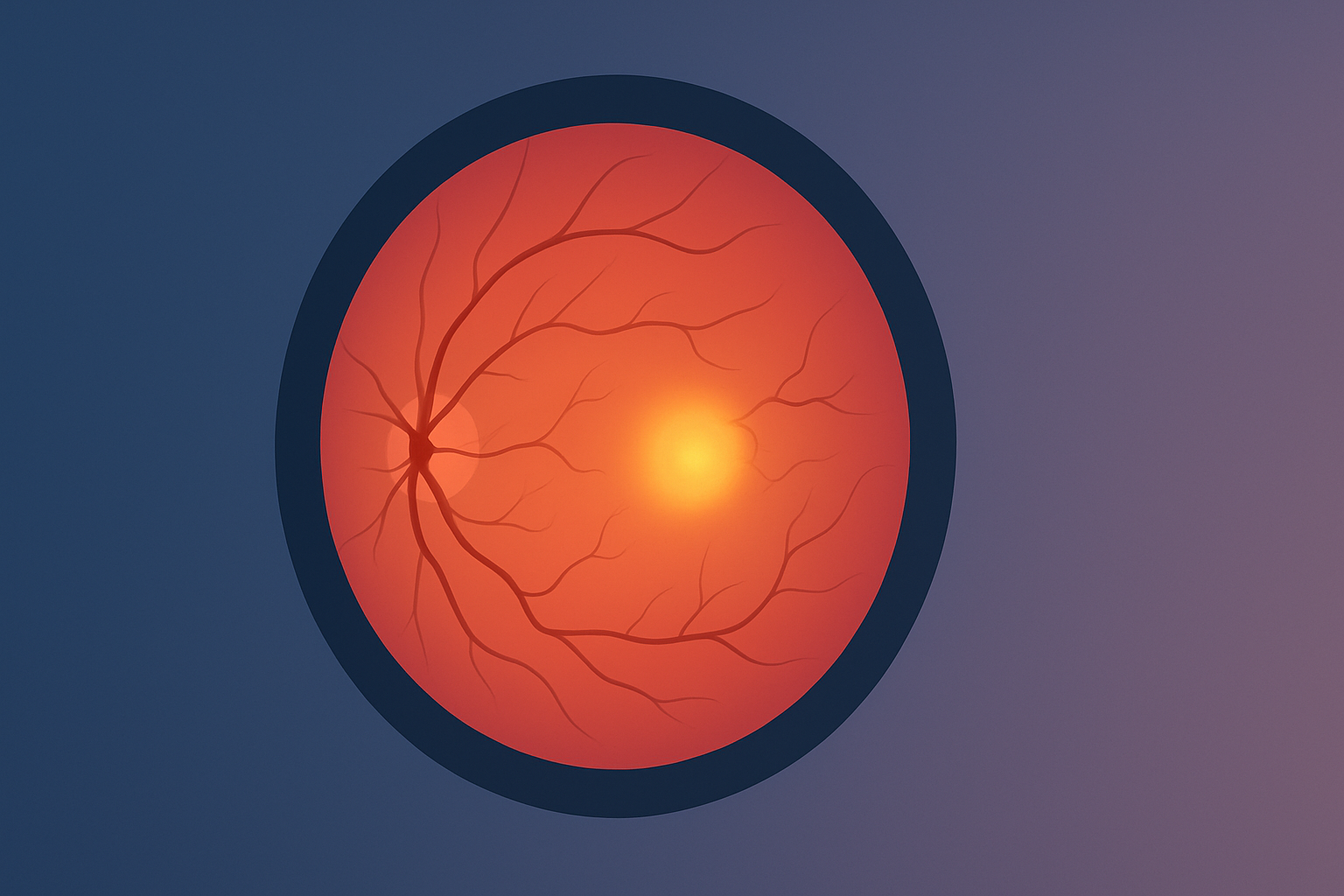
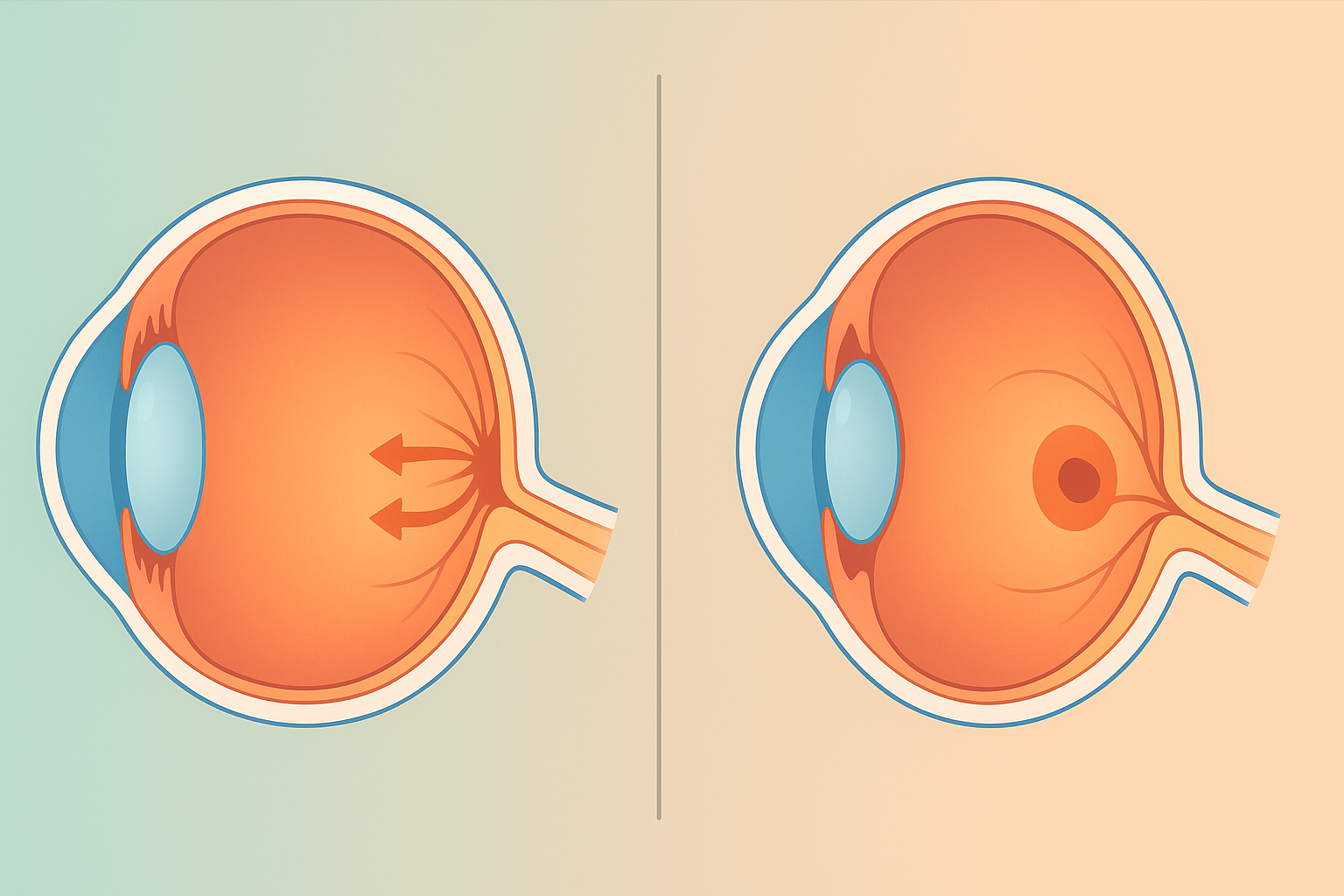
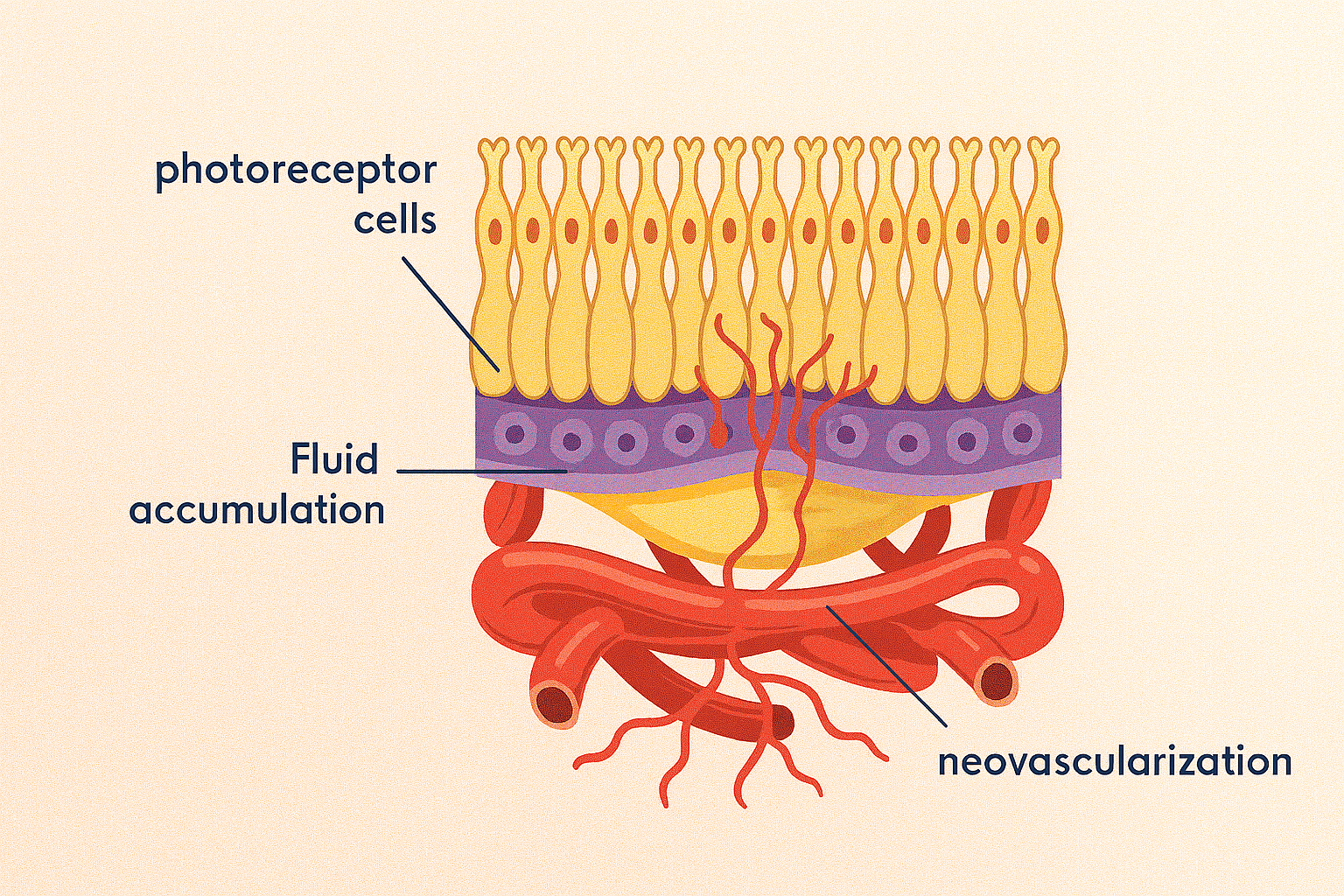
Macular edema is fluid buildup in the macula, the small central area of the retina that enables sharp, color, daylight vision. In cystoid macular edema (CME), tiny fluid pockets collect in a spoke-like pattern within the macula. This leakage typically comes from weakened or inflamed retinal blood vessels and disrupts the way photoreceptors and nerve cells process light. People often describe the view as hazy or as if looking through cellophane. Because the macula is densely packed with cone cells, even mild swelling can noticeably reduce clarity.
Key symptoms and early warning signs
- Blurry or smudged central vision that makes reading and face recognition harder
- Straight lines that look bent or wavy, called metamorphopsia
- Colors that seem faded or washed out
- A gray or dark spot near the center of vision
- Light sensitivity and glare, especially with night driving
- Fluctuating vision that changes through the day
- Sudden worsening of central vision or a new curtain over vision are urgent red flags
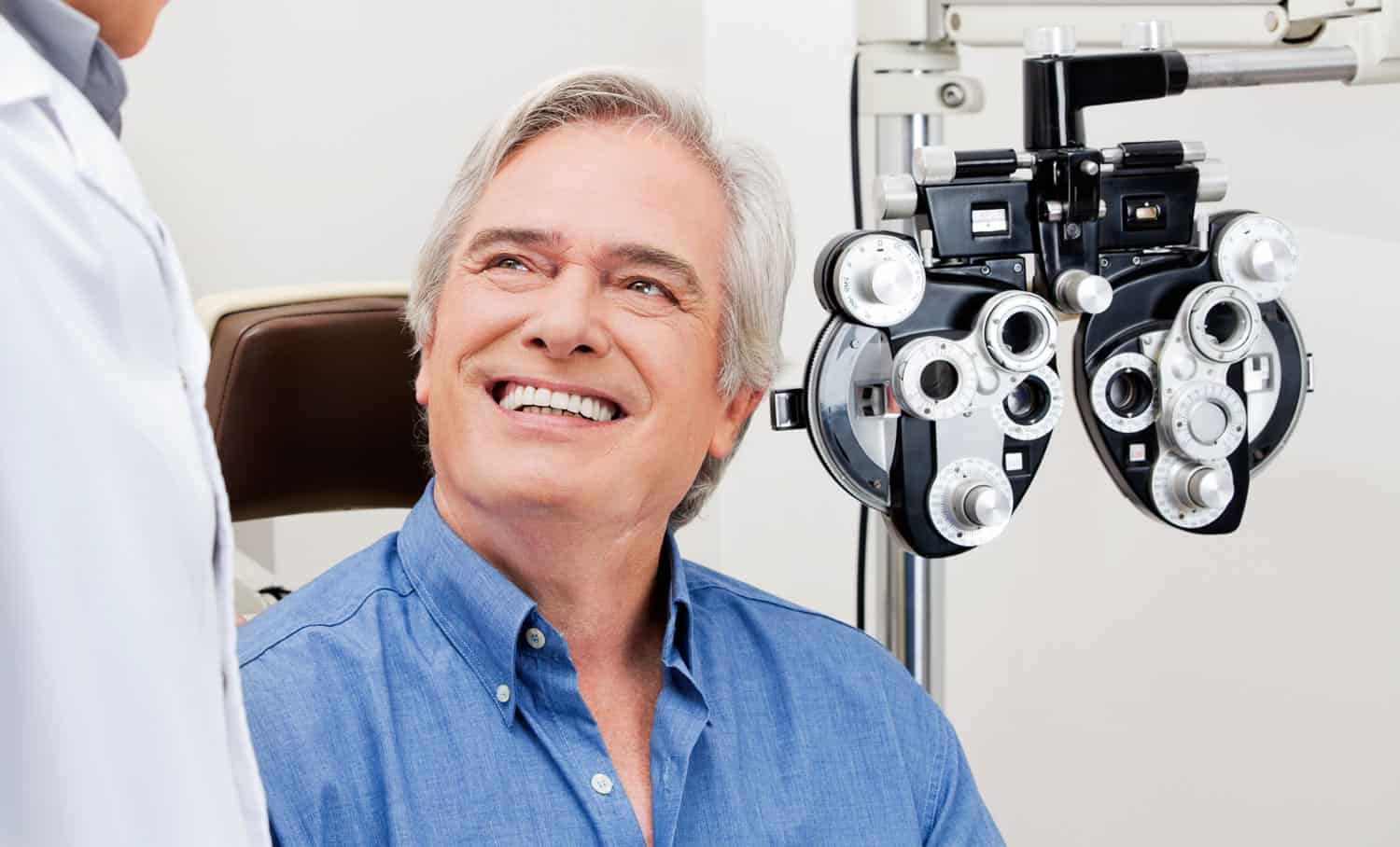
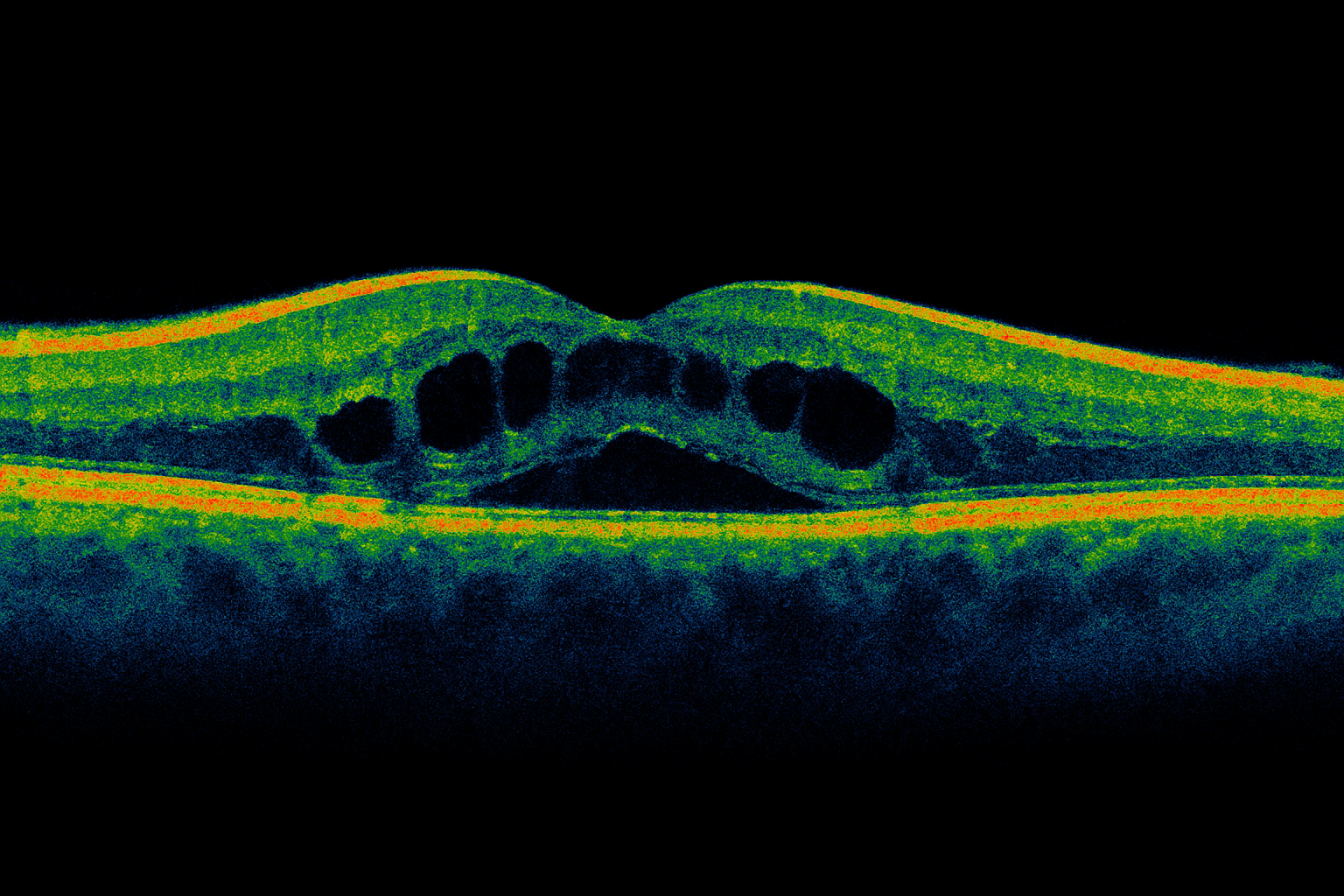
How macular edema is diagnosed
Your eye doctor will dilate the pupils and examine the retina to look for swelling, leakage, or inflammation. Common tests include:
- Optical coherence tomography (OCT) to visualize and measure macular thickness and cystoid changes
- Fluorescein angiography when needed to identify leaking vessels or inflammation patterns
- Visual acuity and Amsler grid to track clarity and distortion over time
- Intraocular pressure and slit-lamp exam to evaluate related eye conditions
- If a systemic issue is suspected, your doctor may coordinate labs or primary care evaluation for blood sugar, blood pressure, or inflammatory markers
Why it happens: causes and risk factors
Macular edema can follow several pathways:
- Diabetes can weaken retinal capillaries and lead to diabetic macular edema
- Retinal vein occlusion and other vascular problems impair normal fluid balance
- Uveitis and other inflammatory conditions promote vessel leakage
- After cataract surgery, temporary CME can occur and often improves with time and drops
- Age-related macular degeneration sometimes includes a swelling component
- Additional risks include uncontrolled hypertension, kidney disease, sleep apnea, smoking, and certain medications
If you are living with diabetes, also see our page on Diabetic Retinopathy. For vascular blockages affecting retinal circulation, see Retinal Occlusion.
Conventional treatment options
The plan depends on cause, severity, and test findings. Your retina specialist may recommend:
- Topical anti-inflammatory drops such as corticosteroids or NSAIDs, commonly used after cataract surgery
- Intravitreal anti-VEGF injections to reduce leakage associated with diabetes or vein occlusion
- Intravitreal steroids or steroid implants when inflammation is prominent or anti-VEGF is insufficient
- Focal or grid laser in selected cases
- Systemic management of blood sugar, blood pressure, lipids, kidney function, and sleep apnea
- Observation for mild post-operative CME that is improving on its own
Many patients require a series of injections over months. Close follow up with OCT helps guide timing and response.
Eye Health Institute’s integrative approach
Our role is to complement your medical and surgical care while working to support retinal circulation, calm inflammation, and promote fluid balance in the macula. Care is individualized and may include:
- Acupuncture targeted to ocular and systemic points to encourage microcirculation and autonomic balance that may help the retina’s fluid regulation
- Micro Acupuncture 48 and electroacupuncture techniques chosen for patients with vascular or inflammatory drivers
- Microcurrent retinal stimulation with clinical devices such as ACS-3000 to gently stimulate retinal tissue and support metabolism during recovery and between medical treatments
- Herbal and nutritional support tailored to your history and medications. This may include omega-3 fatty acids, antioxidants like lutein and zeaxanthin, and botanicals selected to support microvascular health
- Hydrogen therapy and other restorative modalities used in clinic programs to reduce oxidative stress exposure
- Lifestyle coaching focused on steady blood glucose, healthy blood pressure, sleep quality, hydration, and stress resilience
- Intensive programs vs at-home plans based on your travel, schedule, and response, always coordinated with your retina specialist’s recommendations
We avoid anything that could interfere with injections or prescribed drops and coordinate timing so integrative care fits safely around your medical treatments. Our aim is to help stabilize visual function, comfort, and reading endurance while conventional therapy addresses the underlying cause.
What patients report and clinical insights
Patients commonly notice practical gains first. Improvements often show up as:
- Less wavy distortion on the Amsler grid
- Sharper contrast that makes black text stand out better on white backgrounds
- Longer reading or screen stamina before blur creeps in
- Reduced light sensitivity with night driving and bright environments
- More stable day-to-day clarity as swelling trends down on OCT
Every case is different. Outcomes vary by the underlying diagnosis, how long edema has been present, and how the retina responds to injections or drops. In our experience, early integrative support and consistent follow up provide the best chance to preserve function while the macula heals. If edema becomes chronic, the goal shifts to maintaining comfortable, usable vision and preventing further decline.
Self-care foundations that support recovery
These daily choices can make a meaningful difference alongside your medical plan:
- Keep blood sugar in the target range your doctor sets, with steady meals and movement
- Work with your primary care team to optimize blood pressure and cholesterol
- Stay well hydrated unless your medical team advises fluid restriction
- Prioritize sleep and ask about screening for sleep apnea if you snore or feel unrefreshed
- Do not smoke and avoid secondhand smoke
- Wear quality sunglasses to reduce glare and light sensitivity
- Follow all prescribed drops and injection schedules, and bring your medication list to every visit
For background reading on macular anatomy and disease, you may find the National Eye Institute helpful: https://www.nei.nih.gov
When to seek urgent care
Get urgent eye care if you notice any of the following:
- Sudden vision loss or a rapid drop in central clarity
- A curtain or shadow moving over your vision
- Many new floaters with flashes of light
- Severe eye pain, significant redness, or sensitivity to light after surgery or an injection
- Eye trauma of any kind
These symptoms can signal emergencies such as retinal detachment, retinal tears, or severe inflammation and need same-day evaluation. If you cannot reach us quickly, go to the nearest emergency department or call your eye doctor immediately.